Where to Buy Suprep Bowel Prep Kit (and How Much It Costs)

If you’ve received a prescription for the Suprep Bowel Prep Kit, you’re probably facing two questions: where can I buy it, and how much will it cost?
For many Americans, the answer to the second question comes as an unwelcome surprise. With retail prices ranging from $140 to $170 per kit, Suprep represents a significant out-of-pocket expense—especially for uninsured patients or those with high-deductible plans.
Proper bowel preparation is essential for an accurate colonoscopy, yet cost barriers shouldn’t prevent you from completing this life-saving screening.
This guide explains exactly where to purchase Suprep, how much you can expect to pay, and proven strategies to reduce your costs—including prescription discount programs, manufacturer assistance, generic alternatives, and trusted international pharmacy options.
What is the Suprep Bowel Prep Kit?
Suprep Bowel Prep Kit is a prescription medication used to clean your colon before a colonoscopy. It contains three active ingredients—sodium sulfate, potassium sulfate, and magnesium sulfate—that work together as a low-volume, osmotic bowel cleanser.
Unlike older, high-volume bowel preps, Suprep requires drinking a smaller amount of solution, which many people find easier to tolerate.
Suprep is taken in a split-dose regimen, meaning you drink part of the solution the evening before your procedure and the rest on the morning of your colonoscopy. This method helps improve cleansing quality and visibility for your doctor.
Why does proper bowel preparation matter?
Good bowel preparation is essential for an accurate and successful colonoscopy. When your colon is clean, your doctor can:
- Spot and remove polyps more easily
- Detect early signs of colon cancer
- Reduce the need to repeat the procedure
- Avoid cancelled or incomplete exams
Studies show that up to 1 in 4 colonoscopies are affected by inadequate bowel prep. Using a high-quality prep like Suprep—and following the instructions carefully—helps ensure you get the most accurate results.
Prescription requirements
Suprep is not available over the counter. Because it causes fluid and electrolyte shifts in your body, the FDA requires a doctor’s prescription.
To receive Suprep, your healthcare provider will:
- Review your medical history
- Confirm that Suprep is appropriate for you
- Send a prescription to your preferred pharmacy
Most pharmacies keep Suprep in stock, but availability can vary. If you are using a mail-order pharmacy, allow extra time for delivery.
How much does Suprep cost?
Suprep can be expensive in the United States, especially for people without insurance. The typical U.S. retail price ranges from $140 to $170 per kit, though prices can vary depending on your location and the pharmacy’s pricing policies.
Because there is no single standardized price across the country, many people find Suprep unaffordable without assistance or alternative pharmacy options.
Average retail price in the U.S.
Most patients pay between $140 and $170 before insurance. Several factors influence the final cost:
- Regional price differences
- Pharmacy markup policies
- Local wholesale acquisition costs
- Manufacturer price adjustments
Cash price vs. Insurance copay
If you have insurance, your cost depends on your plan’s formulary system. Suprep may be placed on a higher tier, leading to a higher copay, often between $40 and $100.
If you are uninsured—or if your plan doesn’t cover Suprep—your out-of-pocket cost may be close to the full retail price.
Factors that affect your final price
- Whether your insurance requires prior authorization
- Whether your pharmacy has negotiated a lower cost
- Use of coupons, discount cards, or savings programs
- Availability of generic alternatives if your doctor approves them
Insurance coverage for Suprep
Coverage varies across private insurance plans and Medicare Part D. Suprep may be:
- Fully covered
- Partially covered
- Covered only after prior authorization
- Placed on a higher specialty tier (resulting in a higher copay)
If your insurance considers Suprep “non-preferred,” your doctor may need to document why it is medically necessary. Medicare Part D plans may offer coverage, but copays differ widely from one plan to another.
Ways to save on Suprep
There are several ways to reduce your out-of-pocket costs.
Prescription discount cards
Discount programs may help uninsured patients find lower prices. Savings vary by location, pharmacy, and availability.
Manufacturer copay assistance
The manufacturer may offer copay savings for eligible patients with commercial insurance. Patients enrolled in Medicare, Medicaid, or government assistance plans are usually not eligible.
Ask about generic Suprep
A generic formulation containing the same active ingredients (sodium sulfate, potassium sulfate, and magnesium sulfate) may be available. When available, generic versions usually cost significantly less than the brand-name product.
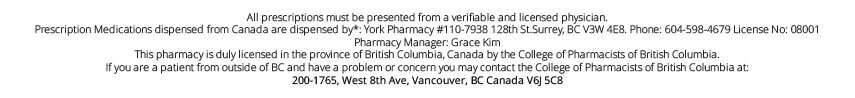
Opt for a Canadian pharmacy
Many Americans find significant savings by purchasing Suprep from a Canadian pharmacy through services like PrescriptionPoint, which connects U.S. patients to licensed international pharmacies. This option can reduce costs substantially compared to U.S. retail prices, with the added convenience of home delivery and dedicated customer support.
Ask your doctor about lower-cost bowel prep alternatives
If the cost of Suprep is too high, your doctor may approve another prep that:
- Works in a similar way
- Is more affordable
- It is covered better by your insurance
Such alternatives may include PEG-based solutions or over-the-counter combinations. Over-the-counter alternatives to Suprep that are often recommended by doctors for colonoscopy prep include regimens using products like MiraLAX, Dulcolax (bisacodyl), magnesium citrate, and sometimes senna.
Safety
While many people tolerate Suprep well, common side effects include:
- Nausea
- Bloating
- Stomach discomfort
- Chills
- Mild vomiting
Less common but serious risks include:
- Severe dehydration
- Electrolyte imbalances
- Heart rhythm disturbances in sensitive patients
People with kidney problems, heart failure, or certain electrolyte disorders should use Suprep only under close medical supervision.
Where to buy the Suprep Bowel Prep Kit
Suprep is available by prescription at:
- Most local community pharmacies across the United States
- Licensed mail-order pharmacies
- Accredited international mail-order pharmacies
Because pricing varies so widely in the U.S., many patients look for trusted, lower-cost alternatives.
Local pharmacies
You can fill your prescription at nearly any neighborhood pharmacy, though prices may vary.
Mail-order pharmacies
Some insurance plans encourage the use of mail-order pharmacies, which may offer stable pricing and home delivery.
International pharmacy option (PrescriptionPoint)
Many Americans choose licensed Canadian mail-order pharmacies such as PrescriptionPoint to save significantly on prescription medications.
Through PrescriptionPoint, you can:
- Order a Suprep Bowel Prep Kit at a lower cost
- Upload your valid prescription
- Receive delivery directly to your home
- Access customer support and order tracking
This option is especially helpful for seniors, uninsured patients, or anyone struggling with the high U.S. retail price.
Buy a Suprep Bowel Kit for $135 from a Canadian pharmacy through PrescriptionPoint.com.
Tips for a smooth purchase
- Ask your doctor to send the prescription early
- Check stock availability before your procedure date
- Allow extra time for shipping if using mail-order
- Bring or upload any discounts or coupons you plan to use
- Confirm your insurance coverage in advance
FAQs
Is Suprep covered by insurance?
Coverage varies. Some plans cover it fully, while others require higher copays or prior authorization.
How much does Suprep cost without insurance?
The average U.S. retail price is typically $140 to $170 per kit.
Why is Suprep so expensive?
Price differences in the U.S. are influenced by insurance contracts, pharmacy markups, wholesale prices, and manufacturer pricing.
Can you buy Suprep over the counter?
No. Suprep is available by prescription only.
Are there cheaper alternatives to Suprep?
Yes. Generic Suprep, PEG-based solutions, and certain OTC regimens may be less expensive. Always ask your doctor before making a switch.
Conclusion
Finding affordable access to the Suprep Bowel Prep Kit doesn’t have to derail your colonoscopy planning.
While U.S. retail prices remain high, you now have a clear roadmap for reducing your costs. Start by comparing local pharmacy prices using discount cards like GoodRx and asking your doctor about generic formulations with the same active ingredients.
For the most significant savings, consider buying Suprep from a Canadian pharmacy through PrescriptionPoint—a trusted service that connects Americans to licensed international pharmacies offering substantially lower prices with home delivery and customer support.
Remember that proper bowel preparation directly affects the quality of your colonoscopy results—incomplete prep can lead to missed polyps, rescheduled procedures, and delayed diagnoses.
Don’t let cost concerns cause you to skip or inadequately prepare for this important screening. Request your prescription early to allow time for price comparisons and shipping (shipping information), discuss all available prep options with your doctor, and use PrescriptionPoint to make Suprep accessible within your budget.
References
- FDA Suprep Bowel Prep Kit Prescribing Information. https://www.accessdata.fda.gov/drugsatfda_docs/label/
- FDA Drug Database Entry for Suprep Bowel Prep Kit. https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm
- Official Suprep Patient Information & Instructions for Use. https://suprepkit.com
- MedlinePlus Drug Summary – Bowel Preps. https://medlineplus.gov/druginformation.html
- GoodRx Suprep Average Retail Price Overview. https://www.goodrx.com
- SingleCare Drug Pricing Database. https://www.singlecare.com
- Mayo Clinic Colonoscopy Prep Resource Page. https://www.mayoclinic.org
- ACG Guidelines for Colorectal Cancer Screening. https://gi.org
- Medicare Drug Coverage overview. https://www.medicare.gov
- How to Make Your Colonoscopy Prep “Not Suck”. https://fightcolorectalcancer.org/blog/how-to-make-your-colonoscopy-prep-not-suck/
Farxiga vs Jardiance: Which SGLT2 Inhibitor Is Right for You?

When managing type 2 diabetes, heart failure, or chronic kidney disease, choosing the right medication can feel overwhelming—especially when you’re navigating insurance coverage and medication costs. Two SGLT2 inhibitors, Farxiga (dapagliflozin) and Jardiance (empagliflozin), have emerged as powerful treatment options that go beyond blood sugar control. This comprehensive guide will help you understand the similarities, differences, and practical considerations between these two medications, empowering you to make informed decisions about your healthcare.
Overview of Farxiga and Jardiance
Farxiga and Jardiance belong to a revolutionary class of diabetes medications called SGLT2 inhibitors (sodium-glucose cotransporter-2 inhibitors). Unlike traditional diabetes drugs that focus solely on insulin or blood sugar, these medications work by blocking a protein in your kidneys that normally reabsorbs glucose back into your bloodstream. Instead, excess glucose is eliminated through urine, providing multiple health benefits beyond diabetes management.
Farxiga (dapagliflozin) was first approved by the FDA in 2014 and has since received additional approvals for heart failure and chronic kidney disease. Manufactured by AstraZeneca, it’s available in 5mg and 10mg tablets and recently became available as a generic medication, making it more affordable for many patients.
Jardiance (empagliflozin), developed by Boehringer Ingelheim and Eli Lilly, received FDA approval in 2014 for the treatment of diabetes and was later approved for additional indications, including heart conditions and kidney disease. Available in 10mg and 25mg strengths, Jardiance remains brand-only, though patient assistance programs can help reduce costs.
The comparison between these medications matters because both have demonstrated remarkable benefits in major clinical trials. They don’t just lower blood sugar—they protect your heart and kidneys while potentially reducing hospitalizations and extending life. For adults over 50, particularly those with multiple health conditions, understanding these differences can be life-changing.
How Farxiga and Jardiance Works
To understand why these medications are so effective, it’s helpful to know how they work in your body. The SGLT2 protein acts like a recycling system in your kidneys, capturing about 90% of the glucose that would otherwise be lost in urine and returning it to your bloodstream. This made sense for our ancestors who faced food scarcity, but in our modern world of abundant calories, this system can work against us.
Both Farxiga and Jardiance block this SGLT2 protein, forcing your kidneys to excrete 60-80 grams of glucose daily through urine. This glucose elimination provides several benefits:
Blood Sugar Improvement: By removing excess glucose, both medications lower A1C levels by 0.5-1.0% when used as monotherapy or added to existing diabetes treatments, according to American Diabetes Association Standards of Care (2023).
Weight Loss: The glucose lost through urine represents approximately 240-320 calories daily, leading to modest but meaningful weight loss of 4-6 pounds over six months for most patients.
Blood Pressure Reduction: The mild diuretic effect and improved blood vessel function typically reduce systolic blood pressure by 2-4 mmHg, providing additional cardiovascular protection.
Heart and Kidney Protection: Beyond these direct effects, SGLT2 inhibitors appear to protect heart muscle cells and kidney cells through mechanisms scientists are still studying, including reduced inflammation and improved cellular energy production.
Key Similarities Between Farxiga and Jardiance
Drug Class and Mechanism
Both medications are SGLT2 inhibitors that block the same protein target in your kidneys. They share the fundamental mechanism of preventing renal glucose reabsorption, leading to glucose excretion through urine. This shared mechanism explains why their benefits and side effect profiles are remarkably similar.
The SGLT2 protein is primarily located in the proximal tubule of your kidneys, where both dapagliflozin and empagliflozin bind reversibly to block glucose reabsorption. This blocking action is dose-dependent, meaning higher doses provide greater glucose elimination, though the relationship isn’t perfectly linear.
Dosing Frequency & Formulations
Both Farxiga and Jardiance offer the convenience of once-daily dosing, typically taken in the morning with or without food. This simple dosing schedule improves medication adherence compared to multiple-daily-dose medications.
Farxiga is available in 5mg and 10mg tablets, with most patients starting at 5mg daily and potentially increasing to 10mg based on tolerance and kidney function. The medication is also available in fixed-dose combinations with metformin (Xigduo XR) and saxagliptin (Qtern).
Jardiance comes in 10mg and 25mg strengths, with 10mg being the typical starting dose for diabetes and heart failure, while 25mg may be used for diabetes management in patients with good kidney function. Fixed-dose combinations include Jardiance with metformin (Synjardy) and with linagliptin (Glyxambi).
Both medications maintain consistent blood levels throughout 24 hours, allowing flexible timing of daily administration. However, taking them at the same time each day optimizes their effectiveness.
Shared Side Effects
The similar mechanism of action between Farxiga and Jardiance results in nearly identical side effect profiles. Understanding these shared risks helps you make informed treatment decisions and know what to monitor.
Genital Yeast Infections: The increased glucose in urine creates an environment that promotes yeast overgrowth. Women experience genital yeast infections in approximately 5-15% of cases, while men may develop balanitis (inflammation of the penis) in 2-4% of cases. Good hygiene and staying well-hydrated can reduce this risk.
Urinary Tract Infections (UTIs): Both medications increase UTI risk by 2-4% compared to placebo. Symptoms include burning during urination, frequent urination, or pelvic pain in women. Adequate fluid intake and proper hygiene help prevent UTIs.
Dehydration and Hypotension: The mild diuretic effect can occasionally lead to dehydration, especially in hot weather, during illness, or with inadequate fluid intake. Signs include dizziness when standing, dry mouth, or decreased urination.
Serious but Rare Risks: Both medications carry black box warnings for rare but serious complications, including diabetic ketoacidosis (even with normal blood sugars), kidney injury, and Fournier’s gangrene (a severe genital infection requiring immediate medical attention).
Critical Differences: Jardiance vs Farxiga
Active Ingredients
While both are SGLT2 inhibitors, the active ingredients differ in their chemical structure and some pharmacological properties.
Dapagliflozin (Farxiga) has a slightly longer half-life of approximately 17 hours and achieves maximum blood concentrations 2-3 hours after dosing. It’s processed primarily by the liver and eliminated through both the kidney and liver pathways.
Empagliflozin (Jardiance) has a shorter half-life of about 12 hours but maintains effective SGLT2 inhibition for 24 hours. It reaches peak levels 1-2 hours after dosing and is eliminated mainly through the kidneys with some liver metabolism.
These pharmacological differences don’t typically translate to clinically meaningful differences in effectiveness or side effects, but they may influence prescribing decisions in patients with severe liver disease.
FDA-Approved Indications
The FDA approvals for these medications have evolved as clinical trial data demonstrated benefits beyond diabetes management.
Farxiga FDA Approvals:
- Type 2 diabetes (adults): Approved 2014
- Heart failure with reduced ejection fraction (HFrEF, adults): Approved 2020
- Chronic kidney disease (adults): Approved 2021
- Heart failure with preserved ejection fraction (HFpEF, adults): Approved 2022
- Type 1 diabetes: Previously approved but withdrawn due to DKA risk
Jardiance FDA Approvals:
- Type 2 diabetes (adults and pediatric patients ≥10 years): Approved 2014
- Heart failure with reduced ejection fraction (HFrEF, adults): Approved 2021
- Chronic kidney disease (adults): Approved 2023
Notably, Jardiance is the only SGLT2 inhibitor approved for pediatric diabetes (children 10 years and older), while Farxiga currently has broader heart failure approvals, including HFpEF.
Generic Availability & Cost Implications
The availability of generic medications can significantly impact your out-of-pocket costs and insurance coverage decisions.
Generic Farxiga (dapagliflozin) became available in early 2024, potentially reducing costs by 80-90% compared to the brand version. Generic availability typically improves insurance coverage and reduces prior authorization requirements.
Brand-Only Jardiance remains under patent protection until approximately 2025-2027. Without generic competition, insurance coverage may require prior authorization or higher copayments. However, manufacturer copay cards can reduce costs for eligible patients.
For uninsured patients, generic dapagliflozin might cost $50-150 per month through discount programs, while brand Jardiance could cost $500-600 monthly without assistance. This price difference makes Farxiga more accessible for many patients on fixed incomes.
How to Take Jardiance vs Farxiga
Type 2 Diabetes
Both medications offer flexible dosing based on your kidney function and treatment response.
Farxiga Diabetes Dosing:
- Starting dose: 5mg once daily in the morning
- Maximum dose: 10mg once daily
- Kidney function requirements: eGFR ≥25 mL/min/1.73m²
- Can be taken with or without food
Jardiance Diabetes Dosing:
- Starting dose: 10mg once daily in the morning
- Maximum dose: 25mg once daily
- Kidney function requirements: eGFR ≥20 mL/min/1.73m²
- Can be taken with or without food
Your doctor may start with lower doses if you have kidney concerns or are taking medications that affect kidney function. Dose increases typically occur after 2-4 weeks if the initial dose is well-tolerated.
Heart Failure (HFrEF and HFpEF)
Heart failure dosing focuses on cardiovascular protection rather than maximum diabetes control.
Farxiga Heart Failure Dosing:
- Standard dose: 10mg once daily
- Used regardless of diabetes status
- Continue unless eGFR falls below 25 mL/min/1.73m²
- Monitor kidney function and volume status
Jardiance Heart Failure Dosing:
- Standard dose: 10mg once daily
- Used in patients with or without diabetes
- Continue unless eGFR falls below 20 mL/min/1.73m²
- Regular monitoring of kidney function is required
Both medications should be continued during heart failure hospitalizations unless acute kidney injury develops. The heart protection benefits occur within weeks of starting treatment.
Chronic Kidney Disease
CKD dosing prioritizes kidney protection while accounting for reduced kidney function.
Farxiga CKD Dosing:
- Standard dose: 10mg once daily
- Used when eGFR 25-75 mL/min/1.73m²
- Continue even as eGFR declines to 25 mL/min/1.73m²
- Monitor for volume depletion
Jardiance CKD Dosing:
- Standard dose: 10mg once daily
- Used when eGFR ≥20 mL/min/1.73m²
- May continue until dialysis initiation
- Regular kidney function monitoring is essential
Both medications slow kidney function decline and may be continued longer than traditional diabetes medications as CKD progresses.
Farxiga vs Jardiance Side Effects
Common Adverse Effects
Understanding common side effects helps you distinguish normal medication effects from serious complications requiring medical attention.
Urogenital Infections (10-15% of patients): Increased glucose in urine promotes bacterial and yeast growth. Women experience more frequent urinary tract infections and vaginal yeast infections. Men may develop balanitis or urinary tract infections. Maintaining good hygiene, staying hydrated, and urinating after sexual activity can reduce infection risk.
Volume Depletion (2-5% of patients): The mild diuretic effect can cause dehydration, particularly in hot weather, during illness with vomiting or diarrhea, or with inadequate fluid intake. Symptoms include dizziness when standing, fatigue, dry mouth, or decreased urination frequency.
Hypoglycemia: When used alone, SGLT2 inhibitors rarely cause low blood sugar. However, when combined with insulin or sulfonylureas, the risk increases. Your doctor may need to reduce doses of these other medications.
Serious Risks
While rare, serious adverse effects require immediate medical attention and careful patient education.
Diabetic Ketoacidosis (DKA): Both medications can trigger DKA even with normal blood glucose levels. Risk factors include severe illness, surgery, prolonged fasting, excessive alcohol intake, or sudden insulin reduction. Symptoms include nausea, vomiting, abdominal pain, difficulty breathing, or fruity breath odor. Stop the medication and seek immediate medical care if DKA is suspected.
Acute Kidney Injury: Dehydration or volume depletion can precipitate kidney injury, particularly in elderly patients or those taking ACE inhibitors or diuretics. Regular kidney function monitoring is essential, especially during illness or medication changes.
Lower Limb Amputations: Clinical trials showed a small increased risk of toe and foot amputations, primarily in patients with existing circulation problems or previous amputations. Good foot care and regular podiatry visits are important for high-risk patients.
Fournier’s Gangrene: This rare but life-threatening genital infection requires emergency surgery. Symptoms include severe genital or perineal pain, swelling, fever, or malaise. Though extremely rare (fewer than 1 in 10,000 patients), immediate medical evaluation is crucial if these symptoms develop.
Special Populations
Elderly Patients: Adults over 65 may experience more frequent side effects, particularly dehydration and impaired kidney function. Starting with lower doses and more frequent monitoring is often recommended.
Pregnancy and Breastfeeding: Neither medication is recommended during pregnancy due to potential kidney effects on the developing fetus. Women planning pregnancy should discuss alternative diabetes treatments with their healthcare provider.
Surgical Procedures: Stop SGLT2 inhibitors 3 days before major surgery or procedures requiring prolonged fasting to reduce DKA risk. Resume after normal eating patterns return and kidney function is stable.
Farxiga vs Jardiance Cost
Retail Prices in the U.S. and Canada
Understanding medication costs helps you budget for long-term treatment and explore savings opportunities.
Average Monthly Costs (in U.S.):
According to online sources, the average price of generic Farxiga at U.S. retail pharmacies typically costs between $330 and $765 for a 30-day supply, depending on the pharmacy chain and dosage.
The average out-of-pocket cost for brand Farxiga at U.S. retail pharmacies ranges from about $580 to $830 for a 30-day supply when purchased without insurance
The average out-of-pocket cost for brand-name Jardiance at U.S. retail pharmacies ranges from about $620 to $875 for a 30-day supply, depending on the pharmacy and location.
Average Monthly Costs (in Canada)
The average price of Farxiga at a Canadian pharmacy through PrescriptionPoint.com is approximately $133 to $256. This means you save between $324 and $697 by purchasing Farxiga from Canada.
Canadian pharmacy pricing through PrescriptionPoint.com offers Jardiance for $54.90 to $328.30, representing potential savings of $291 to $820 compared to purchasing the same medication in the United States.
Generic vs Brand Pricing Impact
The introduction of generic dapagliflozin has created significant cost advantages for Farxiga over Jardiance.
Generic Advantages:
- 80-90% cost reduction compared to the brand
- Improved insurance coverage with fewer restrictions
- Multiple manufacturers are increasing competition and availability
- Pharmacy discount programs offering additional savings
Brand Considerations:
- Consistent manufacturing and appearance
- Some insurance plans may require brand authorization
- Patient assistance programs may provide comparable savings
- Slightly different inactive ingredients rarely affect tolerability
For most patients on fixed incomes, generic dapagliflozin offers the best value proposition, though individual insurance coverage and assistance program eligibility should guide the final decision.
Can You Switch Between Farxiga and Jardiance?
Switching between SGLT2 inhibitors is generally safe and straightforward, though several clinical considerations guide the decision.
Medical Reasons for Switching:
- Cost and insurance coverage changes
- Side effect differences (though rare)
- Specific FDA approvals for your conditions
- Availability issues or pharmacy preferences
Switching Process: Most doctors recommend stopping one SGLT2 inhibitor and starting the other the next day at the equivalent dose. No washout period is typically necessary since both medications have similar mechanisms and kinetics.
Dose Equivalency: While not perfectly equivalent, general conversions include:
- Farxiga 5mg ≈ Jardiance 10mg
- Farxiga 10mg ≈ Jardiance 10-25mg
Your doctor will consider your kidney function, treatment response, and tolerance when determining the appropriate dose of the new medication.
Monitoring After Switching: Continue regular blood sugar, kidney function, and blood pressure monitoring. Most patients experience no difference in effectiveness or side effects when switching, though individual responses may vary.
Farxiga vs Jardiance: Which Is Better for You?
Choosing between Farxiga and Jardiance requires weighing multiple factors specific to your health conditions, financial situation, and treatment preferences.
Choose Farxiga (dapagliflozin) if:
- Cost is a primary concern, and generic availability matters
- You have heart failure with preserved ejection fraction (broader FDA approval)
- You’re comfortable with the DAPA-HF and DAPA-CKD trial data
Choose Jardiance (empagliflozin) if:
- You’re treating pediatric diabetes (the only SGLT2 inhibitor approved for children)
- Your insurance covers brand Jardiance with low copays
- You prefer medications with the largest kidney trial data (EMPA-KIDNEY)
Consider Your Specific Conditions:
- Diabetes only: Either medication is appropriate; cost may be a deciding factor
- Heart failure: Both show similar benefits; Farxiga has HFpEF approval
- Kidney disease: Both provide kidney protection; consider trial data preferences
- Multiple conditions: Either medication addresses all approved indications
Financial Decision Framework:
- Calculate total monthly costs with insurance and assistance programs
- Consider long-term affordability and potential insurance changes
- Factor in monitoring costs and healthcare visits
- Evaluate generic availability and future cost trends
Clinical Decision Factors:
- Your doctor’s experience and comfort with each medication
- Hospital or healthcare system formulary preferences
- Specific trial data that influenced your doctor’s recommendation
- Your response to the previous SGLT2 inhibitor treatment
Frequently Asked Questions
What is better, Jardiance or Farxiga?
Neither medication is definitively “better” than the other. Both are highly effective SGLT2 inhibitors with nearly identical mechanisms of action and clinical benefits. The choice depends on your specific circumstances:
- For cost-conscious patients: Generic Farxiga typically offers better value
- For pediatric diabetes, Jardiance is the only approved option for children
- For heart failure: Both provide similar cardiovascular protection
- For kidney disease: Both offer substantial kidney protection based on large clinical trials
Your healthcare provider will consider your medical conditions, insurance coverage, and individual factors to determine the most appropriate choice.
Can Farxiga cause diarrhea?
Diarrhea is not a common side effect of Farxiga, occurring in fewer than 3% of patients in clinical trials. However, some people may experience gastrointestinal symptoms, including:
- Mild nausea (especially when starting treatment)
- Occasional stomach upset
- Changes in bowel habits
If you experience persistent diarrhea while taking Farxiga, contact your healthcare provider, as it could indicate:
- Dehydration requiring medical attention
- An unrelated illness or infection
- A rare medication reaction requiring evaluation
Most gastrointestinal side effects resolve within the first few weeks of treatment as your body adjusts to the medication.
Why would a doctor prescribe Farxiga?
Doctors prescribe Farxiga for multiple evidence-based reasons beyond diabetes management:
- Cardiovascular Protection
- Kidney Protection
- Diabetes Management
- Multi-condition Treatment
- Safety Profile
What is the downside of Jardiance?
Like all medications, Jardiance has potential disadvantages to consider:
- Cost Factors
- Common Side Effects
- Serious but Rare Risks
- Volume Depletion
- Drug Interactions
- Lifestyle Considerations
Despite these potential downsides, most patients tolerate Jardiance well, and the cardiovascular and kidney benefits often outweigh the risks for appropriate candidates.
Key Takeaways
Similarities: Both Farxiga and Jardiance are highly effective SGLT2 inhibitors offering once-daily convenience, similar side effect profiles, and proven benefits for diabetes, heart failure, and kidney disease. Clinical trial data show comparable cardiovascular and kidney protection between medications.
Key Differences: Generic Farxiga availability provides significant cost advantages, while Jardiance remains brand-only with higher costs but broader pediatric approval. FDA indications vary slightly, with Farxiga approved for both HFrEF and HFpEF, while Jardiance is approved for pediatric diabetes.
Cost Considerations: Generic dapagliflozin costs 80-90% less than brand options, making it more accessible for uninsured or underinsured patients. For additional savings, consider purchasing from licensed Canadian pharmacies through PrescriptionPoint.com, which offers both medications at significantly reduced prices compared to U.S. retail costs.
Clinical Decision: Choose based on your specific conditions, insurance coverage, and financial situation. Both medications provide substantial health benefits, with the “best” choice depending on individual circumstances rather than the superior efficacy of one over the other.
Safety Monitoring: Both medications require regular kidney function monitoring, adequate hydration, and awareness of rare but serious side effects. Stop medication and seek medical care for signs of diabetic ketoacidosis, severe dehydration, or serious infections.
Long-term Perspective: SGLT2 inhibitors represent a paradigm shift in treating diabetes, heart failure, and kidney disease. The cardiovascular and kidney protection benefits often justify their use even in patients without diabetes, making them valuable long-term investments in your health.
For adults over 50 managing multiple chronic conditions on fixed incomes, both Farxiga and Jardiance offer life-extending benefits that extend far beyond blood sugar control. Work closely with your healthcare provider and pharmacist to navigate insurance coverage, assistance programs, and monitoring requirements to ensure you receive optimal treatment within your budget. To explore cost-effective options, you can buy Farxiga online or buy Jardiance online through verified Canadian pharmacy services that may offer substantial savings on your monthly medication costs.
References & Evidence
- McMurray JJV, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. New England Journal of Medicine. 2019;381(21):1995-2008. (DAPA-HF Trial)
- Packer M, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. New England Journal of Medicine. 2020;383(15):1413-1424. (EMPEROR-Reduced Trial)
- Heerspink HJL, et al. Dapagliflozin in patients with chronic kidney disease. New England Journal of Medicine. 2020;383(15):1436-1446. (DAPA-CKD Trial)
- EMPA-KIDNEY Collaborative Group. Empagliflozin in patients with chronic kidney disease. New England Journal of Medicine. 2023;388(2):117-127. (EMPA-KIDNEY Trial)
- American Diabetes Association. Standards of Care in Diabetes—2023. Diabetes Care. 2023;46(Supplement_1).
- Solomon SD, et al. Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. New England Journal of Medicine. 2022;387(12):1089-1098. (DELIVER Trial)
- Anker SD, et al. Empagliflozin in heart failure with a preserved ejection fraction. New England Journal of Medicine. 2021;385(16):1451-1461. (EMPEROR-Preserved Trial)
- FDA Drug Approval Letters and Labels for Farxiga (dapagliflozin) and Jardiance (empagliflozin). Available at: www.fda.gov
- Kidney Disease: Improving Global Outcomes (KDIGO). Clinical Practice Guideline for Diabetes Management in Chronic Kidney Disease. 2022.
- American Heart Association. Heart Failure Clinical Practice Guidelines. 2022 Update.
When to Stop Eliquis Before Tooth Extraction?

Undergoing a tooth extraction while on Eliquis can be nerve-wracking. The fear of bleeding complications may leave you wondering if it’s necessary to stop your blood thinner medication. Unfortunately, the answer isn’t always straightforward. This guide will help you understand when to stop Eliquis before a tooth extraction, including the risks, safety guidelines, and key steps for coordinating with your healthcare team. You’ll learn how to make the safest choice based on your individual medical history, the complexity of the procedure, and your bleeding risks.
Understanding Eliquis (Apixaban)
Eliquis is a widely prescribed blood thinner. It belongs to a class of medications called direct oral anticoagulants (DOACs). These drugs prevent blood clots. They do this by blocking Factor Xa, a key protein in clotting. Understanding how Eliquis works can help. It allows you to make informed decisions about dental procedures.
Apixaban is the generic name for Eliquis. It’s the active ingredient that gives Eliquis its anticoagulant effect.
Doctors commonly prescribe Eliquis for a range of conditions, including:
- Atrial fibrillation (AFib): An irregular heartbeat that increases stroke risk
- Deep vein thrombosis (DVT): Blood clots in leg veins
- Pulmonary embolism (PE): Blood clots in the lung arteries
- Prevention after hip or knee replacement surgery
Pharmacokinetic Properties of Eliquis
Pharmacokinetics is the branch of pharmacology that studies how the body affects a substance, such as a medication, after it is administered. It focuses on the movement of a drug into, through, and out of the body over time, often summarized by the acronym ADME.
- Absorption: How the drug enters the bloodstream from its site of administration.
- Distribution: How the drug spreads throughout the body’s tissues and fluids.
- Metabolism: How the body chemically alters the drug, typically in the liver.
- Excretion: How the drug and its metabolites are eliminated from the body, often via the kidneys in urine or the liver in bile/feces
Understanding how your body processes Eliquis helps determine safe timing for dental procedures.
- Half-life: Eliquis has a half-life of approximately 12 hours. This means your body eliminates half the medication every 12 hours.
- Complete elimination: It takes about 5 half-lives (roughly 60 hours or 2-3 days) for your body to eliminate 95% of the medication.
- Kidney function matters: Your kidneys help eliminate Eliquis. If you have kidney problems, the medication stays in your system longer.
These pharmacokinetic properties are important. They form the basis for the 24–48 hour hold guidelines before certain dental procedures.
Risks Associated with Tooth Extraction on Eliquis
Balancing bleeding and clotting risks is crucial when planning dental extractions.
Bleeding Risk Factors
Several factors increase your bleeding risk during tooth extraction:
- Procedure complexity: Simple single-tooth extractions have a lower bleeding risk. The risk is higher with multiple extractions. It also increases with surgical procedures.
- Number of teeth: Extracting multiple teeth increases bleeding surface area and risk.
- Patient age: Older adults may have slower healing and higher bleeding risk.
- Kidney function: Reduced kidney function means Eliquis stays in your system longer.
- Other medications: Blood thinners, NSAIDs (like ibuprofen), and certain supplements can increase bleeding risk.
Thrombotic Risk Factors
Stopping Eliquis temporarily increases your risk of blood clots:
- Stroke history: Previous strokes indicate higher clotting risk.
- Reason for Eliquis: AFib, DVT, or PE history affects your clotting risk level.
- CHADS₂ score: This CHADS₂ scoring system helps predict stroke risk in AFib patients. Higher scores mean greater risk when stopping anticoagulation.
- Duration of medication: Longer holds increase thrombotic risk.
- Other risk factors: Age over 75, diabetes, heart failure, or hypertension increase clotting risk.
Guidelines for Stopping Eliquis Before Extraction
The decision to stop Eliquis depends on balancing bleeding and clotting risks.
Low-Risk Procedures
Simple extractions often don’t require stopping Eliquis. These include:
- Single tooth extraction
- Simple wisdom tooth removal
- Routine dental surgery with minimal tissue trauma
When continuation is acceptable:
- Your dentist can achieve good local bleeding control
- You have no additional bleeding risk factors
- The extraction site is easily accessible for pressure application
Key local measures for continued therapy:
- Pressure gauze application for 30-45 minutes
- Sutures to close extraction sites
- Hemostatic agents like gelatin sponge
- Tranexamic acid mouthwash
- Detailed post-operative bleeding instructions
Research shows there is no major difference in bleeding. This is true whether DOACs are continued or stopped. The finding applies to simple dental extractions. It holds when proper local measures are used.
Moderate/High-Risk Procedures
Complex extractions may require temporarily stopping Eliquis:
- Multiple tooth extractions (3+ teeth)
- Surgical extractions requiring bone removal
- Impacted wisdom teeth removal
- Extractions in patients with bleeding disorders
Recommended hold times:
- Normal kidney function: Stop 24 hours before procedure
- Moderate kidney impairment: Stop 48 hours before procedure
- Severe kidney impairment: Consult physician for individualized timing
Local Hemostatic Measures During Extraction
Effective local bleeding control reduces the need to stop Eliquis.
Pressure Gauze & Sutures
- Pressure application: Bite down firmly on gauze for 30-45 minutes after extraction. This allows initial clot formation.
- Gauze replacement: Change gauze every 30 minutes if bleeding continues. Avoid frequent checking, which can disrupt clot formation.
- Suture placement: Your dentist may place sutures to bring tissue edges together. This reduces bleeding surface area and promotes healing.
- Suture types: Dissolvable sutures typically dissolve in 7-10 days. Non-dissolvable sutures require removal in 5-7 days.
Hemostatic Agents
There are several common hemostatic agents. These include gelatin sponges and oxidized cellulose. Collagen plugs and bone wax are also used. These materials are placed in the extraction site to help control bleeding. Gelatin sponges and oxidized cellulose are absorbable and support clot formation. Collagen plugs promote platelet aggregation. Bone wax is used sparingly to stop bleeding from bone surfaces.
Tranexamic Acid Mouthwash Protocol
Tranexamic acid is an antifibrinolytic agent. It prevents clot breakdown and reduces bleeding.
Preparation: 10mL of 5% tranexamic acid solution
Usage instructions:
- Rinse gently for 2 minutes
- Do not swallow
- Use 4 times daily for 5-7 days
- Start immediately after extraction
Benefits: Studies show a clear drop in bleeding after extractions. This happens when hemostatic agents are used. The effect is stronger when combined with other local measures.
Contraindications: History of blood clots, kidney disease, or color vision problems may preclude use.
When to Restart Eliquis Post-Extraction
Eliquis should be restarted once bleeding is fully controlled. The extraction site must have a stable clot and no active bleeding. The FDA recommends restarting the medication as soon as adequate hemostasis is achieved. There is no exact timing listed, as it depends on the procedure and how well bleeding is managed. Factors like age, kidney function, and overall stroke or clot risk may also affect timing.
Always follow your dentist’s advice. Talk to your prescribing doctor before restarting Eliquis. Coordination between both is important.
Coordinating Care
Successful management requires coordination between your healthcare providers.
Communicating with Your Dentist and Physician
Consider sharing your full medication list and medical history with both your dentist and physician. It may help to carry a medication alert card that mentions your anticoagulant therapy. In complex situations, coordination between both providers might be useful. It’s a good idea to document any decisions made about stopping or continuing Eliquis. Keeping emergency contact details for both providers can also be helpful.
Patient Checklist Before Extraction
You may consider asking your dentist questions like:
- What type of extraction procedure is planned?
- What local bleeding control measures will be used?
- How long should I expect bleeding after the procedure?
- When should I be concerned about bleeding?
- What pain medications are safe with Eliquis?
You may consider asking your physician questions like:
- What is my stroke/clot risk if I stop Eliquis temporarily?
- Do I need to adjust my Eliquis dose before or after extraction?
- Are there any other medications I should avoid?
- When should I restart my normal Eliquis schedule?
What to tell your dentist before the procedure:
- Complete list of medications and supplements
- Recent lab results (kidney function, INR if available)
- History of bleeding or clotting problems
- Previous dental extraction experiences
- Current health status and recent changes
FAQs on Eliquis and Dental Extractions
Do you need to stop Eliquis before tooth extraction?
It depends on how complex the extraction is. Bleeding and clotting risks also matter. The choice of local hemostatic options plays a role, too. The decision should be made jointly with your dentist and prescribing physician. Simple extractions often don’t require stopping Eliquis if proper local measures are used.
Can I extract my tooth while on blood thinners?
Yes, for simple extractions with appropriate local bleeding control measures. Complex cases may require temporary medication hold and medical consultation. Your dentist will assess the specific procedure and your individual risk factors.
Do I need to go off apixaban before dental surgery?
Low-risk surgeries may not require stopping Eliquis. Moderate to high-risk procedures often need a 24-48 hour hold, adjusted for kidney function. The decision depends on balancing bleeding and clotting risks.
When to restart apixaban after dental extraction?
Typically 6-24 hours post-procedure once bleeding is controlled and hemostasis is stable. High bleeding risk procedures may require longer delays. Coordinate restart timing with your prescribing physician.
How long does 5mg of Eliquis stay in your system?
Eliquis has a half-life of approximately 12 hours. It takes about 2-3 days for 95% elimination from your system. This timeline informs the hold recommendations before dental procedures.
How long before surgery can I stop taking Eliquis?
Stop 24 hours before low-risk procedures and 48 hours before moderate to high-risk procedures. Extend the hold time if you have kidney impairment. Always follow your physician’s specific instructions.
What if I forget to stop Eliquis before my extraction?
Contact your dentist immediately. They may postpone the procedure or proceed with enhanced local bleeding control measures.
Are there alternatives to stopping Eliquis?
Yes, enhanced local hemostatic measures can often allow procedures to proceed without stopping anticoagulation. These include specialized gauze, hemostatic agents, sutures, and tranexamic acid mouthwash.
What pain medications are safe with Eliquis?
Acetaminophen (Tylenol) is generally safe. Avoid NSAIDs like ibuprofen, aspirin, or naproxen, which can increase bleeding risk. Always check with your pharmacist or physician before taking new medications.
How do I know if I’m bleeding too much after extraction?
Contact your dentist if you experience bright red bleeding that doesn’t stop with pressure, blood clots larger than a quarter, or continuous bleeding for more than 6-8 hours after extraction.
Final Takeaway
Remember, dental extractions while on Eliquis need careful planning. Your healthcare team must work together. Good preparation is key. Clear communication helps, too. Most procedures can be done safely. This is possible with continued anticoagulation or short, proper breaks.
Managing your Eliquis therapy doesn’t have to strain your budget. With soaring prescription medication costs, Prescription Point offers an affordable solution to help you maintain consistent treatment. You can order Eliquis from Canada and access the same quality medication at a fraction of the cost, ensuring your anticoagulation therapy remains uninterrupted.
References
- FDA.gov. (2016). HIGHLIGHTS OF PRESCRIBING INFORMATION
- National Library of Medicine. (2024). Apixaban
- National Library of Medicine. (2016). Implications of apixaban for dental treatments
- National Library of Medicine. (2016). Direct Oral Anticoagulants and Bleeding Management Following Tooth Extractions—A Prospective Cohort Study
- National Library of Medicine. (2024). Post-extraction bleeding in patients on direct oral anticoagulants
- National Library of Medicine. (2016). Treating patients on new anticoagulant drugs
- National Library of Medicine. (2017). Dental management of patients taking novel oral anticoagulants (NOAs): Dabigatran
- Ada.org. (2016). Oral Anticoagulant and Antiplatelet Medications and Dental Procedures
- National Library of Medicine. (2023). Perioperative Anticoagulation Management
- National Library of Medicine. (2020). Dental extractions on direct oral anticoagulants vs. warfarin: The DENTST study
- Veterans Health Library. (2025). After a Tooth Extraction: Caring for Your Mouth
- MedlinePlus. (2024). Tooth Extraction
- National Library of Medicine. (2023). Oral Surgery Suturing
- National Library of Medicine. (2023). Sutures And Needles
- National Library of Medicine. (2012). Comparison of the Efficacy of Two Local Haemostatic Agents
- National Library of Medicine. (2025). Tranexamic Acid
- National Library of Medicine. (2021). Prevalence and Knowledge of Potential Interactions between Over-the-Counter Products and Apixaban
Side Effects of Eliquis in the Elderly: Risks, Management & Cost-Saving Tips

Eliquis (apixaban) is a commonly prescribed blood thinner for the older adults. This medication helps prevent dangerous blood clots. It treats atrial fibrillation, deep vein thrombosis, and pulmonary embolism. People over 70 need special attention when taking Eliquis. Age-related changes affect how the body processes medications. Older adults often take multiple drugs, increasing risk of side effects like drug interactions. They also face higher bleeding complications. Understanding Eliquis side effects helps older adults stay safe. This guide covers everything you need to know. We’ll discuss common and serious side effects of eliquis in elderly. You’ll learn management strategies and cost-saving tips.
Why Blood Thinners Are Prescribed to Elderly
Blood thinners become more important as we age. Older adults face increased blood clotting risks due to several factors. Atrial fibrillation is common in older adults. This irregular heartbeat greatly increases the risk of stroke. Eliquis helps reduce that risk by preventing clots from forming in the heart. The elderly also face risks from deep vein thrombosis and pulmonary embolism. Reduced mobility and other health issues make clots more likely. Surgery, hospital stays, and long periods of bed rest add to the danger. Age itself changes blood chemistry. Clotting factors increase naturally over time. The blood vessel walls become less flexible. These changes make dangerous clots more probable. Heart conditions are also more common with age. Heart failure can slow blood flow. Patients with artificial valves often need blood thinners for added protection.
Common Side Effects of Eliquis in the Elderly
Understanding Your Risk Profile
Eliquis (apixaban) is generally well-tolerated by most elderly patients, with studies showing that approximately 15-20% of patients over 65 experience some form of bleeding complications. However, the benefits of stroke prevention typically outweigh the risks for most patients when properly monitored. Higher risk elderly patients include those with:
- Kidney disease or reduced kidney function
- History of bleeding disorders
- Multiple medications (especially other blood thinners, NSAIDs, or certain antibiotics)
- Recent surgery or trauma
- Low body weight (under 132 lbs)
- Age over 80 years
- History of falls or mobility issues
Bleeding-Related Effects
Bleeding is the most common side effect of Eliquis in elderly patients, occurring in approximately 2-4% of patients annually for major bleeding events, and 6-9% for minor bleeding episodes. Side effects typically appear within the first 3 months of treatment but can occur at any time.
Signs and Symptoms of Mild Bleeding
Mild bleeding affects about 6-9% of elderly patients and usually doesn’t require emergency care. These symptoms often improve as your body adjusts to the medication over 4-6 weeks.
- Easy bruising from light pressure or minor bumps.
- Large, dark bruises that heal slowly.
- Frequent or long-lasting nosebleeds.
- Nosebleeds triggered by dry air or mild irritation.
- Prolonged bleeding from small cuts.
- Paper cuts or shaving nicks that take time to stop.
- Bleeding gums during brushing or flossing.
- Gum bleeding even with gentle care.
Signs and Symptoms of Serious Bleeding
Serious bleeding needs immediate medical attention. Even small signs should not be ignored.
- Blood in urine (pink, red, or dark in color)
- Pain while passing urine
- Blood clots in urine
- Blood in stool (bright red or black and tar-like)
- Stomach pain along with bloody stool
- Heavy menstrual bleeding
- Bleeding between periods
- Cuts that bleed and don’t stop
- Weakness or dizziness (possible sign of internal bleeding)
Non-Bleeding Side Effects
Eliquis causes other side effects beyond bleeding. These effects are usually manageable with simple measures.
- Nausea
- Anemia
- Dizziness
- Skin rash
Prevention and Self-Care Tips
Understanding how to minimize bleeding risks is especially important when managing side effects of Eliquis in the elderly. These practical strategies can help reduce bleeding complications while maintaining independence and quality of life.
Shaving with Care: Electric razors provide a safer alternative to manual blades for elderly patients taking Eliquis. The reduced risk of nicks and cuts makes electric shaving particularly valuable for those who experience easy bruising or prolonged bleeding from minor injuries. Many patients find that switching to electric razors significantly decreases their daily bleeding concerns.
Gentle Dental Habits: Since gum bleeding is a common side effect, maintaining proper oral hygiene requires special attention. A soft-bristled toothbrush protects sensitive gums while still providing effective cleaning. Gentle flossing techniques and avoiding aggressive brushing help prevent the minor gum bleeding that can occur more frequently in elderly patients on blood thinners.
Choosing Safe Activities: Physical activity remains important for overall health, but activity selection becomes crucial when managing side effects of Eliquis in elderly patients. Low-impact exercises like walking, swimming, or tai chi provide cardiovascular benefits without the fall risk associated with contact sports. These safer alternatives help maintain fitness while reducing the chance of injuries that could lead to serious bleeding complications.
Keeping the Home Fall-Safe: Environmental modifications play a critical role in preventing the injuries that can cause dangerous bleeding in elderly patients. Installing grab bars in bathrooms, ensuring adequate lighting throughout the home, and removing tripping hazards like loose rugs create a safer living environment. These changes are particularly important for elderly patients who may already have balance concerns that increase their fall risk.
Using Protective Items: Simple protective measures can prevent many minor injuries that lead to bleeding complications. Wearing sturdy gloves during gardening, household cleaning, or kitchen work protects hands from cuts and scrapes. For those who kneel frequently or engage in home maintenance, protective padding for knees and elbows provides an additional safety barrier against the bruising and bleeding that can occur more easily while taking Eliquis.
Serious Side Effects Requiring Immediate Attention
Intracranial Hemorrhage (Brain Bleeding)
Intracranial hemorrhage represents one of the most serious side effects of Eliquis in the elderly, requiring immediate emergency medical attention. The FDA label clearly states that bleeding complications, including brain hemorrhage, can result in severe outcomes such as hospitalization, permanent disability, or death.
Clinical studies have documented cases of brain bleeding in patients taking Eliquis, with elderly patients facing significantly higher risks due to age-related factors and underlying health conditions. The anticoagulant properties of Eliquis increase bleeding risk throughout the body, and the brain is particularly vulnerable due to its rich blood supply and delicate tissue structure.
Critical Warning Signs of Brain Bleeding:
- Sudden, severe headache (often described as “the worst headache of my life”)
- Nausea and vomiting, especially when accompanied by headache
- Lethargy, drowsiness, or altered levels of consciousness
- Seizures (may be convulsive or non-convulsive)
- Focal neurological deficits, such as sudden weakness, numbness, or speech difficulties
- Neck stiffness, particularly indicating subarachnoid bleeding
- Confusion, disorientation, or decreased awareness
- Elevated blood pressure, especially high diastolic readings
- Sudden vision changes or loss
- Loss of coordination or balance
Immediate Action Required: Call 911 immediately if any of these symptoms occur. Do not wait to see if symptoms improve, as brain bleeding can rapidly worsen and become life-threatening.
Thrombocytopenia and Hypotension
Dangerously low platelet count (thrombocytopenia) and low blood pressure (hypotension) are serious complications among the side effects of Eliquis in elderly patients that demand immediate medical intervention.
Thrombocytopenia occurs when blood platelet levels drop significantly below normal ranges. Since platelets are essential for blood clotting, this condition dramatically increases bleeding risk and can make even minor injuries dangerous. In elderly patients taking Eliquis, this creates a particularly hazardous situation where normal clotting mechanisms are severely compromised.
Hypotension often develops as a consequence of significant internal bleeding and represents a medical emergency. When blood pressure drops dangerously low, vital organs may not receive adequate blood flow, leading to organ failure.
Warning Signs to Watch For:
- Unusual fatigue or weakness
- Rapid heartbeat or palpitations
- Dizziness or fainting, especially when standing
- Shortness of breath
- Excessive bruising or bleeding from minor injuries
- Pale skin or nail beds
- Cold, clammy skin
- Confusion or altered mental state
While these complications are relatively rare, they require immediate emergency medical attention due to their potentially life-threatening nature.
Allergic Reactions
Serious allergic reactions to Eliquis, though uncommon, can occur at any time during treatment and represent true medical emergencies. The FDA specifically warns about the risk of allergic swelling (angioedema) and anaphylaxis in patients taking Eliquis.
Allergic Swelling (Angioedema): This condition involves rapid swelling of deeper skin layers, particularly around the face, lips, tongue, throat, and airways. When swelling occurs in the throat or tongue, it can quickly obstruct breathing and become life-threatening.
Anaphylaxis: This represents the most severe form of allergic reaction, characterized by a rapid, whole-body response that can cause cardiovascular collapse and death within minutes if not treated immediately.
Emergency Warning Signs:
- Swelling of face, lips, tongue, or throat
- Difficulty breathing or swallowing
- Rapid pulse or dizziness
- Widespread skin rash or hives
- Severe itching
- Nausea, vomiting, or diarrhea
- Loss of consciousness
- Feeling of impending doom
Critical Response: These reactions require immediate emergency medical treatment with epinephrine and other life-saving medications. Call 911 immediately and inform emergency responders that the patient is experiencing a suspected allergic reaction to Eliquis.
Important Note: Allergic reactions can occur even after taking Eliquis successfully for weeks or months. Previous tolerance of the medication does not guarantee continued safety, making awareness of these warning signs crucial throughout the entire treatment period.
Dosing, Administration, and Monitoring in Older Adults
Recommended Dosage and Adjustments
The standard dose of Eliquis is 5 mg taken twice a day. Some patients may need a lower dose of 2.5 mg twice a day. This reduced dose is advised if they meet at least two of these conditions: age 80 or older, body weight of 60 kg or less, or serum creatinine of 1.5 mg/dL or more. These factors can lead to higher levels of the drug in the body. Older adults often process medications differently. The lower dose helps reduce the risk of bleeding in such patients.
Clinical Surveillance in Elderly Patients
Routine lab monitoring is not needed with Eliquis. However, regular clinical checks are recommended. These help spot any signs of bleeding or side effects. This is especially important for older patients. They may have a higher risk of bleeding due to other health conditions or medications. Ongoing assessment helps catch problems early. It also supports the safe, long-term use of the drug.
Monitoring Renal Function
Monitoring kidney function is important during treatment with Eliquis, especially in older adults. Changes in kidney function can affect how the drug works and how safe it is. In patients with poor kidney function, a lower dose may be needed. This depends on their age and body weight. Regular checks of serum creatinine help guide dosing decisions. These checks also ensure that kidney function stays within a safe range during treatment.
Drug Interactions and Polypharmacy Considerations
Elderly patients often take multiple medications. Drug interactions with Eliquis can be dangerous.
Eliquis levels increase with certain antifungals and antibiotics
Drugs like ketoconazole, itraconazole, ritonavir, and clarithromycin increase the amount of Eliquis in the body. These are strong inhibitors of CYP3A4 and P-gp. If a patient is taking Eliquis 5 mg twice daily, the dose should be reduced to 2.5 mg twice daily. If the patient is already on 2.5 mg twice daily, these drugs should be avoided.
Eliquis levels decrease with some seizures and herbal medicines
Rifampin, carbamazepine, and St. John’s wort can lower the levels of Eliquis. These drugs are strong inducers of CYP3A4 and P-gp. Their use with Eliquis should be avoided because they may reduce its effectiveness.
Bleeding risk increases with other blood thinners
Using Eliquis with other anticoagulants or antiplatelet drugs can increase the risk of bleeding. This includes medications like aspirin or warfarin. Such combinations should be used with caution, especially in elderly patients.
Eliquis does not affect how other drugs work
Eliquis does not significantly affect the breakdown of other drugs. It does not strongly inhibit or induce CYP enzymes or P-gp. This means it is unlikely to change how other medications act in the body.
Consider having your medications reviewed regularly. Bring all medications to appointments. Include over-the-counter drugs and supplements.
Balancing Fall Risk and Stroke Prevention
Falls can cause serious brain bleeding in older adults on blood thinners like Eliquis. According to the CDC, head injuries in anticoagulated elders require close monitoring for delayed bleeding or TBI symptoms. However, a PMC review highlights that, for those aged ≥75, apixaban reduces stroke risk significantly and causes fewer brain bleeds compared to warfarin. Thus, the benefit of stroke prevention with apixaban typically outweighs the risk of fall-related bleeding. Fall risk should be managed, but anticoagulation should generally continue, with careful monitoring after any head injury.
Affordability & Access: Cost-Saving Strategies
Eliquis costs create a significant financial burden for many older adults. There are a few ways that could help lower medication expenses.
Licensed Canadian Pharmacies
According to a Canadian government report, U.S. prices for patented medicines like Eliquis are much higher than in Canada. Because of this, some patients may consider licensed Canadian pharmacies. These pharmacies could be a potential option for those looking to reduce their costs. However, a valid U.S. prescription is still required. Use trusted services like PrescriptionPoint.com, which provides verified Canadian pharmacy access. This service helps locate legitimate suppliers. Always check for proper licensing. Avoid unverified online sources.
Patient Assistance Programs
Several programs may help lower the cost of Eliquis for some patients. Drug companies like Bristol Myers Squibb might offer assistance based on income. Discount cards such as GoodRx can offer savings at many pharmacies. Medicare coverage depends on the plan, and some may have high costs during gap periods. State programs might support low-income older adults.
Comparing Eliquis with Other Anticoagulants in Older Adults
Warfarin vs DOACs
Warfarin has a narrow therapeutic window and requires frequent monitoring. DOACs work faster, have more predictable effects, and need less follow-up. In older adults aged ≥75, DOACs match warfarin in preventing stroke and death. They cause fewer intracranial bleeds. However, bleeding risk, especially gastrointestinal, varies by DOAC type; apixaban and edoxaban are safest.
Apixaban vs Rivaroxaban & Dabigatran
Eliquis (apixaban) may be safer than other blood thinners like rivaroxaban and dabigatran. All three drugs work equally well to prevent stroke in people with atrial fibrillation. But Eliquis causes less major bleeding. In one study, it showed a 50% lower risk of major bleeding than dabigatran and a 61% lower risk than rivaroxaban. Rivaroxaban had the highest risk of bleeding, including bleeding in the brain. This makes Eliquis a safer choice for many older adults who are at higher risk of bleeding problems.
FAQs
What is the safest blood thinner for the elderly?
NOACs (Novel Oral Anticoagulants) like apixaban demonstrate at least equal effectiveness to warfarin while offering significantly lower bleeding risks, making them particularly suitable for elderly patients. Apixaban consistently shows the most favorable safety profile among available options, with reduced rates of major bleeding complications. However, the optimal choice depends on several individual factors including kidney function, potential drug interactions, and personal bleeding risk assessment. Healthcare providers carefully evaluate these factors when selecting the most appropriate anticoagulant for each elderly patient.
How long can you be on Eliquis?
Treatment duration with Eliquis varies significantly based on the underlying condition being treated. For patients with atrial fibrillation, treatment is typically lifelong to maintain continuous stroke prevention benefits. For those being treated for deep vein thrombosis (DVT) or pulmonary embolism (PE), the standard treatment course ranges from 3-6 months, though some patients may require extended therapy. Your healthcare provider will determine the most appropriate duration based on your specific medical condition, risk factors, and treatment response.
What is the most common side effect of Eliquis?
Bleeding represents the most frequently reported side effect of Eliquis, occurring across a spectrum from minor bruising and nosebleeds to potentially serious hemorrhagic events. Understanding the side effects of Eliquis in the elderly is particularly important, as older patients may experience more pronounced bleeding tendencies due to age-related factors such as increased fall risk, multiple medications, and underlying health conditions. Additionally, nausea and anemia are commonly reported side effects that patients should discuss with their healthcare providers, especially if these symptoms persist or worsen over time.
What are the long-term side effects of blood thinners?
The primary long-term concern with blood thinners like Eliquis is the cumulative bleeding risk that continues throughout the treatment period. Unlike some medications that may develop new adverse effects with prolonged use, chronic apixaban therapy does not introduce entirely new side effect profiles beyond the known bleeding risks. However, the side effects of Eliquis in elderly patients may become more pronounced over time due to age-related changes in metabolism, kidney function, and overall health status. Regular monitoring helps healthcare providers manage these ongoing risks effectively.
What is the life expectancy of someone on blood thinners?
DOACs like apixaban have been shown to significantly improve patient outcomes by reducing the incidence of stroke and major bleeding events compared to traditional anticoagulants. Clinical studies demonstrate that patients taking apixaban experience approximately a 10% reduction in all-cause mortality compared to those taking warfarin. This improvement in survival rates reflects the medication’s ability to prevent life-threatening cardiovascular events while maintaining a more favorable safety profile. The overall impact on life expectancy depends on individual patient factors and the underlying condition being treated.
What is the best blood thinner with the least side effects?
Among the available DOACs, apixaban consistently demonstrates the lowest risk of gastrointestinal bleeding, making it particularly attractive for patients concerned about digestive system complications. Additionally, apixaban shows significantly lower rates of intracranial hemorrhage compared to warfarin, which is especially important for older adults who may be at higher risk for brain bleeding. However, the determination of the “best” blood thinner must always consider individual patient factors, including kidney function, drug interactions, adherence capabilities, and personal bleeding risk profile. Healthcare providers work with patients to select the most appropriate anticoagulant based on these personalized considerations.
Final Takeaway
This comprehensive guide helps people older than 70 and caregivers understand Eliquis use safely. Regular communication with healthcare providers ensures optimal treatment outcomes. Cost-saving strategies make treatment more affordable for older adults on fixed incomes, and services like Prescription Point offer additional solutions to combat soaring prescription medication costs by providing access to affordable medications from licensed Canadian pharmacies.
For those seeking cost-effective options, you can buy Eliquis from Canada through our trusted online pharmacy services. Remember that individual medical decisions require professional consultation. This information supplements but doesn’t replace medical advice. Always discuss treatment options with qualified healthcare providers.
References
- FDA.gov. (2012). Highlights of Prescribing Information
- National Library of Medicine. (2013). Anticoagulation in Patients Aged ≥75 years with Atrial Fibrillation: Role of Novel Oral Anticoagulants
- National Library of Medicine. (2014). Efficacy and safety of apixaban compared with warfarin according to age for stroke prevention in atrial fibrillation: observations from the ARISTOTLE trial
- National Library of Medicine. (2022). Pathophysiological Aspects of Aging in Venous Thromboembolism: An Update
- CDC.gov. (2024). About Atrial Fibrillation
- National Library of Medicine. (2022). Deep Venous Thrombosis and Pulmonary Embolism Secondary to Mild Traumatic Injury in an Elderly Male With No Additional Risk Factors
- National Library of Medicine. (2008). Hemostasis and ageing
- CDC.gov. (2024). About Heart Failure
- National Library of Medicine. (2025). In brief: What are anticoagulants?
- ISMP.org. (2018). Eliquis is a high alert medicine.
- National Library of Medicine. (2024). Intracranial Hemorrhage
- CDC.gov. (2024). Information for Health Care Providers
- National Library of Medicine. (2015). Stroke prevention in the elderly atrial fibrillation patient with comorbid conditions: focus on non-vitamin K antagonist oral anticoagulants
- CMS.gov. (2024). Medicare Drug Price Negotiation Program: Negotiated Prices for Initial Price Applicability Year 2026
- Health Canada. (2023). Annual Report 2021
- Health Canada. (2021). Choosing a safe online pharmacy
- BMSPAF.org. (2025). We provide certain Bristol Myers Squibb medicines to eligible patients free of charge
- GoodRx. (2025). Compare eliquis prices in U.S.
- Medicare.gov. (2025). How much does Medicare drug coverage cost?
- NCSL.org. (2022). State Pharmaceutical Assistance Programs
- National Library of Medicine. (2022). Effectiveness and Safety of DOACs vs. Warfarin in Patients With Atrial Fibrillation and Frailty: A Systematic Review and Meta-Analysis
- National Library of Medicine. (2016). Direct Comparison of Dabigatran, Rivaroxaban, and Apixaban for Effectiveness and Safety in Nonvalvular Atrial Fibrillation
- National Library of Medicine. (2022). Comparison of the Efficacy and Safety of Apixaban and Warfarin in the Prevention of Stroke in Patients With Non-valvular Atrial Fibrillation: A Meta-Analysis
Step-by-Step Guide to Safely Buying Eliquis from Canada with a Prescription from Your U.S. Doctor

Prescription drug prices in the U.S. are higher than in many other countries. To reduce costs, the U.S. launched programs to import drugs from Canada. The goal is to make medications more affordable for American patients. The FDA’s rule points to high U.S. drug prices. These prices are driving cross-border sourcing. This suggests some Americans may turn to Canadian pharmacies for affordable medications.
Canadian pharmacies offer significant savings on life-saving medications like Eliquis. But is it safe to buy Eliquis from Canada? Buying Eliquis from a licensed Canadian pharmacy may be safe and legal under certain conditions, such as when a valid prescription is provided and the pharmacy complies with regulations..
Licensed Canadian pharmacies dispense drugs that meet Health Canada’s safety standards. Yet, choosing the right pharmacy is crucial for your safety. This comprehensive guide walks you through everything you need to know. We’ll cover safety protocols, legal considerations, and step-by-step ordering instructions. You’ll also learn how to identify legitimate pharmacies and avoid dangerous counterfeits.
What Is Eliquis (Apixaban)?
Eliquis is a brand-name blood thinner containing the active ingredient apixaban. It belongs to a class of medications called direct oral anticoagulants (DOACs). These drugs prevent dangerous blood clots.
The medication has revolutionized blood clot prevention since its FDA approval in 2012. Unlike older blood thinners like warfarin, Eliquis doesn’t require frequent blood monitoring. This makes it more convenient for patients and doctors alike.
Approved Uses & Administration
Eliquis treats several serious conditions:
- Atrial fibrillation (irregular heartbeat) to prevent stroke
- Deep vein thrombosis (DVT) treatment and prevention
- Pulmonary embolism treatment and prevention
- Post-surgical blood clot prevention
Standard dosing varies by condition. Most patients take 5mg twice daily for atrial fibrillation. DVT and pulmonary embolism treatment usually begins with 10mg twice a day for seven days. After that, the dose reduces to 5mg twice daily. Your doctor sets the dose based on your condition, age, weight, and kidney function. Never adjust your dose without medical supervision. Take Eliquis with or without food at the same time each day.
Mechanism of Action
Eliquis works by blocking Factor Xa, a key protein in the blood clotting process. When Factor Xa is inhibited, your blood takes longer to clot. This prevents dangerous clots from forming in your blood vessels. The drug is highly selective for Factor Xa. This specificity reduces the risk of excessive bleeding compared to older anticoagulants. However, all blood thinners carry some bleeding risk. Eliquis reaches peak blood levels within 3-4 hours after taking a dose. The medication stays active in your system for about 12 hours. This is why most patients take it twice daily.
Common Side Effects & Risks
The most serious risk with Eliquis is bleeding. This can range from minor bruising to life-threatening internal bleeding. Seek immediate medical attention for signs of serious bleeding:
- Unusual bruising or bleeding
- Blood in urine or stool
- Vomiting blood or coffee-ground material
- Severe headache or dizziness
- Weakness or fainting
Common mild side effects include:
- Easy bruising
- Minor bleeding (nosebleeds, gum bleeding)
- Nausea
- Skin rash
Tell your doctor about all medications and supplements you take. Some drugs increase bleeding risk when combined with Eliquis. Never stop taking Eliquis without medical supervision, as this increases stroke risk.
Why Consider Buying Eliquis from Canada?
Canadian pharmacies may present affordable options for U.S. patients facing high medication costs. The potential benefits could extend beyond just lower prices.
Cheaper Medications
The price difference can be huge. The official list price for a 30-day supply of Eliquis is $606. However, many U.S. pharmacies sell a 30-day supply of 5mg Eliquis for around $700 to $750 according to various price comparison sites.
The PMPRB, an independent board under Health Canada tracks drug prices through its CompassRx report. In one 2018 to 2019 edition, brand-name Eliquis was listed at 146.88 Canadian dollars. That is about 110 to 120 US dollars.
PrescriptionPoint partners with licensed pharmacies that require valid prescriptions and follow appropriate safety protocols in accordance with Canadian law. We offer a 30-day supply of brand-name Eliquis 5mg for approximately $70—some licensed Canadian pharmacies may offer lower prices for Eliquis compared to U.S. retail prices. However, prices vary and may not include shipping or handling fees.
If you’re looking for an even more affordable option, the generic version, apixaban, is also available and typically ranges between $60 and $100 per month through our service.
These savings come from Canada’s drug pricing rules. The Patented Medicine Prices Review Board (PMPRB) enforces them. It is an independent body that reports to Parliament. The board sets maximum prices for new patented drugs. Companies must follow these limits. This keeps medicine prices lower in Canada. Brand drug prices are 2.78 times higher in the U.S. than in Canada, according to the Government Accountability Office.
Canadian Medication Standards and Safety
While Canadian medications are regulated by Health Canada, aiming for high standards of safety and effectiveness, it’s always wise to verify the specific product and source. Their approval process mirrors FDA requirements.
Generic medications must prove bioequivalence to brand-name drugs. This means they work identically in your body. Health Canada’s standards for generics match or exceed U.S. requirements.
Manufacturing facilities are subject to regular inspections, and quality control measures are in place to help ensure the consistent strength and quality of medications. Canadian pharmacies licensed by provincial regulatory bodies are required to follow Health Canada’s standards for drug quality and safety.
Convenience, Privacy & Access
Canadian pharmacies offer discreet home delivery throughout the U.S. Most orders arrive within 2-3 weeks via standard mail. Express shipping options are available for urgent needs. Packaging is discreet with no identifying marks about the contents. This protects your medical privacy during delivery. Most pharmacies use secure, tamper-evident packaging.
For uninsured Americans, Canadian pharmacies provide access to essential medications. You don’t need insurance coverage to order. Payment options include credit cards, bank transfers, and money orders.
Is It Legal to Import Eliquis from Canada?
The rules around importing prescription drugs can be complex. In some cases, it may be allowed for personal use. Checking FDA guidelines and state laws can help with understanding the process.
FDA Personal Importation Policy
According to FDA laws and/or regulations, importation of medications for personal use may be considered, although generally prohibited, under specific conditions where the FDA may allow exceptions.
- The medication is for personal use only (up to 90-day supply).
- You have a valid U.S. prescription.
- The drug is not available in the U.S.
- The medication is not a controlled substance.
- The product doesn’t pose unreasonable health risks.
People often import to save money, but the FDA doesn’t permit it for that reason. The FDA’s approach to personal importation is outlined in its guidelines.. Their focus is on commercial importers and dangerous products.
U.S. and State-Level Importation Laws
Several U.S. states are exploring prescription import programs. Florida launched the first approved one in 2023. These aim to cut costs for state health programs. Some rules apply to personal imports. It’s best to check with a doctor or pharmacist.
How to Choose a Legitimate Canadian Pharmacy
Selecting a reputable Canadian pharmacy is crucial for your safety. Several verification methods help identify legitimate providers.
Licensing & Provincial Regulation
All legitimate Canadian pharmacies must be licensed by their provincial pharmacy regulatory body. Each province maintains a public database of licensed pharmacies. Verify your chosen pharmacy appears in these official listings.
Key provincial regulators include:
- Ontario College of Pharmacists
- College of Pharmacists of British Columbia
- Alberta College of Pharmacy
- College of Pharmacists of Manitoba
Check the pharmacy’s license number against the official database. Legitimate pharmacies prominently display their license information on their websites.
CIPA & IPABC Certification
The Canadian International Pharmacy Association (CIPA) provides additional verification. CIPA members must meet strict standards for licensing, prescription requirements, and patient safety. Look for the CIPA seal on pharmacy websites. CIPA pharmacies have served over 10 million U.S. patients since 2002 with a perfect safety record, according to CIPA.com. This demonstrates the reliability of certified providers. The International Pharmacy Association of British Columbia (IPABC) offers similar certification for B.C.based pharmacies. Their members follow enhanced safety protocols and quality standards.
Prescription & Contact Requirements
Legitimate pharmacies always require valid prescriptions from licensed U.S. doctors. They never sell prescription medications without proper documentation. Be wary of any pharmacy offering to sell prescription drugs without a prescription.
Reputable pharmacies provide clear contact information, including:
- Physical address in Canada.
- Licensed pharmacist available for consultation.
- Secure website with SSL encryption.
How to Buy Eliquis from Canada: Step-by-Step
Buying Eliquis from a Canadian pharmacy may involve a few basic steps. This process is often followed by people looking to import medications. Here’s how to buy Eliquis from Canada through Prescriptionpoint.com
Obtain and Submit Your Prescription
If you’re planning to import Eliquis for personal use, you need a valid prescription from a U.S. doctor. Make sure to include any required documents. This could be a letter from your physician. It should explain why you need the medication.
The FDA may allow a 90-day supply. But this is only under certain conditions. Submit your prescription through our secure online portal. We accept digital photos or scanned copies.
It may be a good idea to include accurate contact details and a shipping address when placing an order. Adding a phone number could help if we need to reach out. Double-checking the information might help avoid any issues.
Pharmacist Review & Consultation
A licensed Canadian pharmacist reviews every prescription before it is filled. This helps ensure the medication and dosage are correct. The review is required by Canadian pharmacy regulations. Patients can ask questions about their medication. The pharmacist will give advice to support safe and proper use. These services are only offered by licensed pharmacies that follow national standards.
Payment, Shipping & Customs
Canadian pharmacies often accept payments like personal checks, certified checks, e-checks, and money orders. Credit cards may not always be accepted. Shipping to the U.S. usually takes 2 to 4 weeks. Costs can vary depending on the order. Sometimes shipments are delayed by customs inspections. If customs contacts you, giving them a valid prescription and saying the medicine is for personal use usually helps. Some pharmacies follow this process.
Cost Comparison: Canada vs. U.S. Pharmacies
The following table shows typical monthly costs for Eliquis:
| Medication | U.S. Price | Canadian Price | Savings |
| Brand Eliquis 5mg (60 tablets) | US$700-$900 | US$60-$70 approximately | US$630-$840 |
| Brand Eliquis 2.5mg (60 tablets) | US$700-$900 | US$80-$90 approximately | US$610-$820 |
*Prices as on July 2025.
Risks & How to Avoid Counterfeits
While legitimate Canadian pharmacies are safe, counterfeit drug risks exist online. Recognizing warning signs protects your health and money.
Recognizing Rogue Sites
Illegitimate online pharmacies often share common characteristics:
- No prescription required for prescription medications.
- Prices too good to be true (90% below market rates).
- No verifiable physical address or phone number.
- Websites with poor English or obvious grammatical errors.
- Unsolicited email advertisements.
- No licensed pharmacist available for consultation.
These sites often sell counterfeit or contaminated medications. Products may contain wrong ingredients, incorrect dosages, or harmful contaminants.
Health Canada Seizure Data
Health Canada regularly seizes counterfeit medications entering the country. Their enforcement actions target fake versions of popular drugs including blood thinners.
Common counterfeit drug problems include:
- Wrong active ingredient or dosage
- Contamination with harmful substances
- Poor manufacturing quality
- Expired or degraded medications
Stick to licensed, certified pharmacies to avoid these risks. The small additional cost is worth your safety and peace of mind.
Alternatives to Eliquis & Assistance Programs
Some people look into other options to manage costs. These might include alternative treatments or assistance programs.
Other DOACs & Warfarin
Other direct oral anticoagulants include:
- Xarelto (rivaroxaban): Taken once daily for most conditions.
- Pradaxa (dabigatran): Requires twice-daily dosing.
- Savaysa (edoxaban): Once-daily dosing.
Warfarin remains an effective, inexpensive option. However, it requires regular blood monitoring and dietary restrictions.
Discuss these alternatives with your doctor. The best choice depends on your specific condition, other medications, and personal preferences.
Co-pay Cards & Patient Aid
Bristol Myers Squibb offers an Eliquis co-pay card for eligible patients. This can reduce monthly costs to $10 for commercially insured patients. Income and insurance restrictions apply.
Patient assistance programs may provide free medications for qualifying low-income patients. Applications require financial documentation and doctor approval.
You can compare U.S. programs with Canadian prices. Some people find long-term savings through Canadian pharmacies. It depends on your needs and what you’re eligible for.
Related Post – Eliquis Alternatives: Comparing Costs, Safety & Side Effects
FAQs
Where is Eliquis Made?
Eliquis tablets are FDA‑approved, but may be labeled as made in locations such as Puerto Rico, Ireland, Switzerland, or Turkey. DA import checks ensure any source meets U.S. cGMP quality and safety standards
Is Canadian generic Eliquis safe?
Yes, when purchased from licensed pharmacies. Health Canada uses rigorous safety and bioequivalence standards. Verify pharmacy licensing through provincial bodies or CIPA certification. Always use a valid prescription.
What is the price of Eliquis in Canada?
The price of Eliquis in Canada is around $70 for a 30-day supply of the 5mg brand version.
Can prescription medication be mailed from Canada to the U.S.?
The FDA generally does not allow drug imports. However, it may permit a 90-day supply for personal use.
Is Canadian pharmacy service legitimate?
Licensed Canadian pharmacies are legitimate and safe. Confirm licensing by provincial pharmacy authorities. Look for CIPA or IPABC accreditation. Ensure they require prescriptions and provide pharmacist consultation.
Is generic Eliquis as good as brand Eliquis?
Yes, generic apixaban is bioequivalent to brand Eliquis. It meets the same quality and effectiveness standards. Generic versions offer significant cost savings without compromising safety or efficacy.
How long does shipping take from Canada?
Standard shipping typically takes 2-4 weeks via Canada Post to USPS.
Do I need to notify my doctor about ordering from Canada?
Yes, inform your doctor about your medication source. This ensures proper medical record keeping and allows them to monitor your treatment effectively. Most doctors support cost-saving measures for patients.
When will generic Eliquis be available in the U.S.?
FDA approved the first generics of apixaban in Dec 2019. However, the brand holder extended patent rights. Court rulings push availability to April 2028. Once launched, generics should cost significantly less—some estimate under $100/month.
Conclusion and Next Steps
Ordering Eliquis from Canada often provides substantial savings, and it’s generally considered safe if you take the time to research your source or consult with your doctor.. The key is to choose a trusted, certified provider and follow the proper procedures. PrescriptionPoint.com is a CIPA-certified Canadian pharmacy partner that offers affordable pricing on brand-name and generic medications. You can buy Eliquis from Canada through our secure platform and have it shipped directly to your door. We recommend speaking with your doctor about Canadian pharmacy options. They can help provide the appropriate prescription and monitor your treatment.
For Americans on fixed incomes and patients facing high U.S. drug prices, Canadian pharmacies like PrescriptionPoint offer access to life-saving medications at more manageable costs. With the right precautions, this can be a safe, effective, and reliable cost-saving strategy. Take the next step by discussing options with your healthcare provider and exploring certified Canadian pharmacies. Your health and financial peace of mind are worth it.
References
- CMS.gov. (2023). A Report in Response to the Executive Order on Lowering Prescription Drug Costs for Americans
- FDA.gov. (2019). Importation of Prescription Drugs
- CMS.gov. (2023). Transcript: Eliquis, October 30, 2023 Medicare Drug Price Negotiation Program Patient-Focused Listening Session
- Health Canada. (2025). Guidance Document: Regulatory Requirements for Drug Identification Numbers (DINs)
- Health Canada. (2021). Choosing a safe online pharmacy
- FDA.gov. (2012). HIGHLIGHTS OF PRESCRIBING INFORMATION
- National Library of Medicine. (2018). Efficacy and Safety of Apixaban, Dabigatran, Rivaroxaban, and Warfarin in Asians With Nonvalvular Atrial Fibrillation
- Eliquis. (2024). How Much Does ELIQUIS Cost?
- GoodRx. (2025). Eliquis
- Health Canada. (2018). CompassRx, 6th Edition
- Prescription Point. (2025). Are you Looking to Buy Eliquis (Apixaban) from PrescriptionPoint.
- Health Canada. (2023). CompassRx, 9th Edition
- Health Canada. (2024). Regulatory Process
- GAO.gov. (2021). Prescription Drugs: U.S. Prices for Selected Brand Drugs Were Higher on Average than Prices in Australia, Canada, and France
- Health Canada. (2015). How Drugs are Reviewed in Canada
- Health Canada. (2024). Access to Generic Drugs in Canada
- Health Canada. (2024). Good manufacturing practice
- Health Canada. (2024). Drug Identification Number (DIN)
- FDA.gov. (2024). Personal Importation
- FDA.gov. (2025). Importation Program under Section 804 of the FD&C Act
- FDA.gov. (2024). FDA Authorizes Florida’s Drug Importation Program
- NAPRA.ca. (2024). Pharmacy Regulatory Authorities
- CIPA.com. (2024). Licensed, Certified, Trusted
- CIPA.com. (2024). Canadian International Pharmacy Association
- IPABC. (2025). About Us
- Pharmaserve.com. (2025). How to Order
- Health Canada. (2021). Choosing a safe online pharmacy
- FDA.gov. (2025). Counterfeit Medicine
- FDA.gov. (2025). How to Buy Medicines Safely From an Online Pharmacy
- Health Canada. (2025). Buying health products online? Know the risks
- National Library of Medicine. (2017). Direct Oral Anticoagulants: A Quick Guide
- FDA.gov. (2021). Highlights of Prescribing Information
- FDA.gov. (2024). Highlights of Prescribing Information
- FDA.gov. (2015). Highlights of Prescribing Information
- National Library of Medicine. (2022). Cost-effectiveness of Direct Oral Anticoagulant vs. Warfarin Among Atrial Fibrillation Patients With Intermediate Stroke Risk
- Eliquis.bms.com. (2025). ELIQUIS $10 Co-pay Card
- Medicare.gov. (2025). Help with Drug Costs
- National Library of Medicine. (2023). Design and evaluation of oral formulation for apixaban
Why is Gemtesa So Expensive and How to Find Financial Relief

If you’ve been prescribed Gemtesa for overactive bladder, you may have experienced sticker shock at the pharmacy. With a list price of around $552 for a 30-day supply, Gemtesa ranks among the more expensive overactive bladder medications available today. For many Americans, especially those on fixed incomes, high Gemtesa costs can make treatment feel out of reach. But why is Gemtesa so expensive? And more importantly, what can you do to reduce these costs? This guide will help you understand the factors behind Gemtesa’s pricing and explore practical ways to make this medication more affordable.
What Is Gemtesa?
Gemtesa is the brand name for vibegron, a prescription medication used to treat overactive bladder (OAB) in adults. The FDA approved Gemtesa in December 2020, making it one of the newer options for managing OAB symptoms like frequent urination, urgency, and incontinence.
What makes Gemtesa different from other OAB medications is how it works. Vibegron belongs to a class of drugs called beta-3 adrenergic agonists. These medications target specific receptors in the bladder muscle, helping it relax and hold more urine. This mechanism is different from anticholinergic medications like oxybutynin, which can cause more side effects like dry mouth and constipation.
Approximately 33 million U.S. adults have overactive bladder, according to the Urology Care Foundation. This large patient population represents a significant market for pharmaceutical companies developing OAB treatments. Gemtesa was developed by Urovant Sciences and is now marketed by Sumitomo Pharma America.
The medication comes as a 75 mg tablet taken once daily with or without food. Clinical trials showed that Gemtesa can reduce the average number of daily bathroom trips and accidents in people with overactive bladder.
Factors Contributing to Gemtesa’s High Cost
Understanding why Gemtesa costs so much requires looking at the complex factors that influence drug pricing. Multiple elements contribute to the high price tag, from initial development costs to marketing expenses.
Research & Development Costs
The journey from laboratory to pharmacy shelf is long and expensive. On average, it costs between $1 billion and $2.8 billion to develop a new drug, according to research published in JAMA. This massive investment includes not just the successful drug, but also the many failed candidates that never make it to market.
For every drug that receives FDA approval, pharmaceutical companies typically test hundreds or thousands of potential compounds. Most of these fail at various stages of development. The companies must recoup these losses through the successful medications they bring to market.
Vibegron’s development took years of research to identify the compound, understand how it works, and optimize its formulation. Scientists had to prove it was both safe and effective before moving to human testing. All of this research requires significant financial investment in laboratories, equipment, and skilled researchers.
Clinical Trial Expenses
Before the FDA approves any new medication, it must undergo rigorous clinical testing. Gemtesa’s pivotal trial, called EMPOWUR, enrolled over 1,500 participants across multiple sites. Clinical trials of this size are extremely expensive to conduct.
The EMPOWUR trial was a Phase 3 study lasting 12 weeks, with participants randomly assigned to receive either Gemtesa or a placebo. Managing a trial of this scope requires hiring research coordinators, monitoring patient safety, collecting and analyzing data, and ensuring regulatory compliance.
Each participant in a clinical trial represents significant costs. The company must pay research sites, compensate participants for their time, and cover medical monitoring. When you multiply these costs across thousands of participants and multiple trial phases, the expenses add up quickly.
Patent Protection & Market Exclusivity
When a pharmaceutical company develops a new drug, they receive patent protection that prevents generic competition for a specific period. Brand-name drugs can have up to 20 years of patent exclusivity from the time they file their initial patent application.
Additionally, new chemical entities (NCEs) like vibegron receive 5 years of data exclusivity from the FDA. This means even if the patent expires, generic manufacturers cannot use the original company’s safety and effectiveness data to get their own approval for 5 years.
This exclusivity period allows companies to set higher prices without generic competition. Once patents expire and generics enter the market, prices typically drop significantly. However, Gemtesa is still relatively new, so generic versions are not yet available.
Marketing & Advertising Spending
Pharmaceutical companies spend billions on marketing their products to both healthcare providers and consumers. In 2022, U.S. direct-to-consumer pharmaceutical advertising totaled $8.07 billion, according to Statista.
You’ve likely seen Gemtesa advertisements on television or in magazines. These marketing campaigns are expensive to produce and air. The company also employs sales representatives who visit doctors’ offices to educate healthcare providers about the medication’s benefits.
Professional medical education, conference sponsorships, and clinical research presentations all represent additional marketing costs. While these activities can provide valuable medical education, they also contribute to the overall cost of bringing a medication to market.
Manufacturing & Quality Control
Producing pharmaceutical-grade medications requires specialized facilities that meet strict FDA standards. These manufacturing plants must maintain precise environmental controls, use high-quality raw materials, and follow detailed quality control procedures.
Every batch of Gemtesa must undergo extensive testing before release to ensure it meets specifications for potency, purity, and safety. This quality control process requires sophisticated laboratory equipment and trained personnel.
The manufacturing facilities themselves represent significant capital investments. Companies must build or lease specialized production lines, install monitoring systems, and maintain backup capabilities to ensure consistent supply.
Regulatory Approval Process
Getting FDA approval involves substantial fees and administrative costs. The FDA charges user fees for new drug applications, which can exceed $3 million for a standard application. These fees help fund the FDA’s review process but add to the overall development costs.
Beyond the initial approval, companies must continue to pay annual fees to maintain their drug’s approval status. They must also fund post-market safety monitoring and submit regular safety reports to the FDA.
Regulatory compliance requires dedicated staff to manage FDA communications, maintain required documentation, and ensure ongoing adherence to safety regulations. These operational costs continue throughout the product’s lifecycle.
PBM & Insurance Negotiations
The drug pricing landscape involves complex negotiations between pharmaceutical companies and pharmacy benefit managers (PBMs). These middlemen manage prescription benefits for insurance companies and negotiate rebates with drug manufacturers.
While the list price (called the Wholesale Acquisition Cost or WAC) for Gemtesa might be $552, the actual amount paid often differs significantly due to rebates and discounts negotiated behind closed doors. However, patients often pay based on the list price, not the discounted net price.
This system can result in patients paying more out-of-pocket while insurance companies and PBMs receive substantial rebates. The complexity of this system contributes to the disconnect between list prices and actual treatment costs.
Perceived Innovation & Value
As a newer medication with a different mechanism of action, Gemtesa is positioned as an innovative treatment option. The beta-3 agonist class may cause fewer anticholinergic side effects compared to older OAB medications.
This perceived advantage allows the manufacturer to command premium pricing. Healthcare providers and patients may be willing to pay more for a medication that offers improved tolerability or effectiveness compared to existing options.
The value proposition extends beyond just treating symptoms to potentially improving quality of life with fewer bothersome side effects. This positioning supports higher pricing in the marketplace.
How Gemtesa’s List Price Is Determined
Understanding how pharmaceutical companies set prices requires distinguishing between different pricing concepts and how they affect what patients actually pay.
Wholesale Acquisition Cost vs. Net Price
The Wholesale Acquisition Cost (WAC) represents the list price that pharmacies pay to acquire medications from manufacturers. For Gemtesa 75 mg (30 tablets), the WAC is approximately $552. This is the “sticker price” you’ll often see quoted.
However, the net price – what’s actually paid after rebates and discounts – is typically much lower. Insurance companies and PBMs negotiate substantial rebates that can reduce the effective price by 20-50% or more. Unfortunately, patients rarely benefit directly from these hidden discounts.
The WAC serves as the starting point for most pricing calculations, including insurance copays and deductibles. This means patients often pay based on the higher list price, even though the actual transaction price is lower.
Insurance Coverage & Out-of-Pocket Costs
Most insurance plans cover Gemtesa, but your out-of-pocket costs depend on your specific plan details. If you have a copay-based plan, you might pay a fixed amount like $30-50 per month. With coinsurance, you pay a percentage of the drug’s cost, perhaps 20-30%.
High-deductible health plans require you to pay the full price until you meet your annual deductible. This can mean paying the entire $552 monthly cost early in the year, which creates a significant financial burden for many patients.
Your plan’s formulary (list of covered medications) also affects costs. If Gemtesa is on a higher tier, your copay will be larger. Some plans may not cover it at all without prior authorization.
Medicare & Medicaid Coverage
Medicare Part D coverage for Gemtesa varies by plan. Most plans include it on their formularies, but it’s typically placed on higher tiers with larger copays. During the coverage gap (donut hole), you may pay up to 25% of the drug’s cost.
Medicare patients might face prior authorization requirements, meaning your doctor must prove medical necessity before coverage begins. This process can delay treatment and create additional administrative burden.
Medicaid coverage differs by state, but most state programs cover Gemtesa with prior authorization. The approval process typically requires trying and failing other, less expensive OAB medications first.
Prior Authorization & Step Therapy
Many insurance plans require prior authorization for Gemtesa, meaning your doctor must submit paperwork justifying the prescription before coverage begins. This process can take several days to weeks.
Step therapy requirements mandate trying less expensive alternatives first. You might need to fail treatment with generic medications like oxybutynin or tolterodine before insurance will cover Gemtesa.
These administrative hurdles are designed to control costs by steering patients toward less expensive options. While this can delay access to preferred treatments, understanding these requirements helps you and your doctor navigate the approval process more effectively.
Gemtesa vs. Other OAB Medications
Comparing Gemtesa to other overactive bladder treatments helps put its cost in perspective and may reveal more affordable alternatives.
Gemtesa vs. Myrbetriq
Myrbetriq (mirabegron) is another beta-3 agonist that works similarly to Gemtesa. Both medications target the same receptors and have comparable effectiveness for OAB symptoms.
Myrbetriq has been available since 2012 and costs approximately $400-450 for a 30-day supply – somewhat less than Gemtesa but still expensive. Generic mirabegron became available in 2023, offering a more affordable alternative with prices around $100-200 per month.
The choice between these medications often comes down to individual response and side effect profiles. Some patients tolerate one better than the other, making the higher cost worthwhile if it provides better symptom control.
Brand-Name vs. Generic OAB Drugs
Generic OAB medications cost significantly less than brand-name options. Generic oxybutynin, for example, costs $10-30 per month compared to hundreds for newer branded medications.
The trade-off is that older generic medications often cause more side effects. Anticholinergics like oxybutynin can cause dry mouth, constipation, and cognitive effects that may be particularly problematic for older adults.
Newer medications like Gemtesa were developed specifically to avoid these side effects, which justifies some of the price difference. However, not everyone experiences troublesome side effects with generic options, making them worth trying first.
Non-Drug Alternatives
Behavioral therapies and lifestyle modifications can effectively manage OAB symptoms without medication costs. Pelvic floor exercises, bladder training, and dietary changes may reduce symptoms significantly.
Physical therapy specifically focused on pelvic floor dysfunction can be highly effective. While this involves upfront costs, it may provide long-term symptom relief without ongoing medication expenses.
Combining behavioral approaches with less expensive medications often provides good results at lower overall costs. Your healthcare provider can help develop a comprehensive treatment plan that balances effectiveness with affordability.
Ways to Reduce Gemtesa Costs
Several strategies can help make Gemtesa more affordable, from manufacturer programs to insurance optimization.
Gemtesa Go Savings Program
Urovant Sciences offers the Gemtesa Go savings program for eligible patients. With this co-pay card, commercially insured patients may pay as little as $10 per month for their prescription. The program has income restrictions and doesn’t cover patients with government insurance like Medicare or Medicaid. You must have commercial insurance and meet other eligibility criteria to qualify. To enroll, visit the manufacturer’s website or ask your pharmacist about the program. The savings card can be used at most pharmacies and significantly reduces your monthly out-of-pocket costs.
Prescription Discount Cards
Services like GoodRx, SingleCare, and Optum Perks offer discount cards that can reduce Gemtesa’s cost even without insurance. These programs negotiate discounted rates with pharmacies and pass some savings to consumers. GoodRx, for example, might offer Gemtesa for $400-450 instead of the full $552 list price. While this is still expensive, it represents meaningful savings for uninsured patients or those with high deductibles. These discount programs are free to use and don’t require enrollment or income verification. Simply present the discount card or app at the pharmacy to receive the negotiated price.
Patient Assistance Programs
Several organizations offer patient assistance programs for those who cannot afford their medications. NeedyMeds maintains a comprehensive database of available programs and eligibility requirements. The Medicine Assistance Tool from the Partnership for Prescription Assistance helps patients find programs that match their specific situations. These programs may provide free or reduced-cost medications to qualifying individuals. Income limits vary by program, but many are designed to help middle-income patients who don’t qualify for Medicaid but still struggle with medication costs. Applications typically require documentation of income and insurance status.
Mail-Order & 90-Day Supply
Many insurance plans offer lower per-pill costs when you order 90-day supplies through mail-order pharmacies. This can reduce your effective monthly cost and minimize trips to the pharmacy.
A 90-day supply might cost $150 instead of $50 for three separate 30-day fills, creating modest but meaningful savings. Check with your insurance plan to see if this option is available.
Mail-order pharmacies also often provide better customer service for managing prior authorizations and insurance issues. They have dedicated teams to handle these administrative challenges.
Insurance Appeals & Formulary Exceptions
If your insurance doesn’t cover Gemtesa or places it on a high-cost tier, you can appeal this decision. Your doctor can request a formulary exception based on medical necessity. The appeals process requires documentation of why Gemtesa is medically necessary compared to covered alternatives. This might include failed trials of other medications or specific side effect concerns. While appeals take time and effort, they’re often successful when properly documented. Your doctor’s office may have staff experienced in managing these requests.
Canadian Online Pharmacies like PrescriptionPoint
For Americans facing high out-of-pocket costs for Gemtesa, licensed Canadian online pharmacies such as PrescriptionPoint.com offer a reliable, lower-cost alternative. By sourcing medications from Canada and overseas with regulated drug pricing, PrescriptionPoint helps U.S. customers access the same prescription drugs—often at significantly reduced prices. This is especially helpful for those without insurance or with high-deductible plans. Ordering through a trusted Canadian pharmacy can be a safe and affordable option to manage ongoing medication expenses.
Frequently Asked Questions
Is Gemtesa covered by Medicare?
Most Medicare Part D plans cover Gemtesa, but it’s typically placed on higher tiers with larger copays. You may need prior authorization, and during the coverage gap, you’ll pay a percentage of the drug’s cost. Check your specific plan’s formulary to understand your coverage details.
How much is a 30-day supply of Gemtesa?
The list price for a 30-day supply of Gemtesa 75 mg is approximately $552. However, your actual cost depends on insurance coverage, available discounts, and manufacturer programs. With the Gemtesa Go program, eligible patients may pay as little as $10 per month.
When will Gemtesa be available as a generic?
Generic versions of Gemtesa are not expected to be available for several years due to patent protection and data exclusivity. The medication received FDA approval in 2020, and new chemical entities typically receive 5 years of data exclusivity plus additional patent protection.
Is Gemtesa worth the money?
This depends on your individual situation and response to treatment. If you’ve tried less expensive alternatives without success or experienced intolerable side effects, Gemtesa’s higher cost may be justified. Discuss the cost-benefit analysis with your healthcare provider.
How can I get Gemtesa cheaper?
Several options can reduce costs: the manufacturer’s Gemtesa Go savings program, prescription discount cards like GoodRx, patient assistance programs, 90-day supplies, insurance appeals and Canadian online pharmacies like PrescriptionPoint.com. Start with the manufacturer program if you have commercial insurance, as this often provides the greatest savings.
Next Steps
If you’re struggling with Gemtesa’s cost, don’t give up on treatment. Start by discussing your financial concerns with your healthcare provider. They may be able to help you access manufacturer programs, apply for patient assistance, or find alternative treatments that fit your budget.
Contact your pharmacist as well – they often have extensive knowledge about available discount programs and can help you navigate different options. Many pharmacies also offer their own discount programs or can direct you to helpful resources.
Check with your insurance company about formulary exceptions or appeals processes. Sometimes a simple phone call can clarify coverage options or identify steps to improve your benefits.
Remember that managing overactive bladder effectively improves your quality of life significantly. While the costs can be challenging, various programs and strategies can make treatment more affordable. The key is exploring all available options and working with your healthcare team to find a solution that works for both your symptoms and your budget.
Another option worth exploring is PrescriptionPoint.com, an affordable destination for Gemtesa and other prescription medications. We offer competitive pricing and provide additional savings opportunities beyond traditional U.S. pharmacies. You can check our current gemtesa price in canada to compare costs and see if this option works for your situation.
With persistence and the right approach, you can find ways to make Gemtesa more affordable while effectively managing your overactive bladder symptoms.
References
- FDA.gov. (2024). Gemtesa Prescribing Information
- FDA.gov. (2020). Drug Trials Snapshot: GEMTESA
- Urologyhealth.org. (2024). What is Overactive Bladder (OAB)?
- Jamanetwork.com. (2016). Fewer Opioids, More Exercise for Severe Joint Pain From Arthritis
- Clinicaltrials.gov. (2021). A Study to Examine the Safety and Efficacy of a New Drug in Patients With Symptoms of Overactive Bladder (OAB) (Empowur)
- FDA.gov. (2020). Frequently Asked Questions on Patents and Exclusivity
- Drugs.com. (2025). Prices, Coupons, Copay Cards & Patient Assistance
- FDA.gov. (2017). Myrbetriq Prescribing Information
- Drugs.com. (2025). Generic Myrbetriq Availability
- Gemtesa.com. (2025). SIGN UP FOR INFO ON SAVINGS AND GEMTESA
Eliquis Alternatives: Comparing Costs, Safety & Side Effects

Blood thinners have become essential medications for millions of Americans, with approximately 6 million people living with atrial fibrillation (AFib) – a number projected to reach 12.1 million by 2030 according to the CDC. Additionally, up to 900,000 U.S. cases of deep vein thrombosis (DVT) and pulmonary embolism (PE) occur annually, resulting in 60,000–100,000 deaths. While Eliquis has emerged as a leading anticoagulant, generating $12.2 billion in revenue for Bristol-Meyers Squibb in 2023, its high cost leaves many patients searching for affordable alternatives.
For seniors on fixed incomes, uninsured adults, and those exploring cross-border pharmacy options, understanding Eliquis alternatives becomes crucial for maintaining both health and financial stability. This comprehensive guide examines FDA-approved alternatives, their costs, safety profiles, and practical switching strategies.
What Is Eliquis?
Eliquis (apixaban) is a direct oral anticoagulant (DOAC) that belongs to a class of medications called Factor Xa inhibitors. Unlike traditional blood thinners like warfarin, which work through the vitamin K pathway, apixaban directly blocks Factor Xa, a key enzyme in the blood clotting cascade. This targeted mechanism helps prevent dangerous blood clots while potentially reducing bleeding risks compared to older anticoagulants.
The FDA has approved Eliquis for several critical indications. In patients with non-valvular atrial fibrillation, it reduces the risk of stroke and systemic embolism. For those who have experienced deep vein thrombosis or pulmonary embolism, Eliquis helps prevent recurrence. The medication is also approved for preventing DVT and PE in patients undergoing hip or knee replacement surgery.
Eliquis works by inhibiting both free and clot-bound Factor Xa, effectively interrupting the coagulation cascade at a crucial step. This mechanism allows for predictable anticoagulation without the need for routine blood monitoring, unlike warfarin which requires regular INR testing. The medication reaches peak blood levels within 3-4 hours and has a half-life of approximately 12 hours, necessitating twice-daily dosing.
Why Consider Alternatives?
Several compelling reasons drive patients to explore eliquis alternatives beyond the brand-name medication. Cost represents the primary concern for many Americans, particularly those without comprehensive insurance coverage. A 30-day supply of Eliquis 5 mg tablets costs between $787 at retail pharmacies, compared to generic warfarin at approximately $4 for the same period.
Bleeding complications, while less common with Eliquis than warfarin, still occur and may prompt physicians to consider alternative anticoagulation strategies. Some patients experience gastrointestinal bleeding, nosebleeds, or excessive bruising that interferes with their quality of life. Additionally, the twice-daily dosing requirement may pose challenges for patients with memory issues or complex medication regimens.
Insurance coverage limitations often force patients to explore different options. Some health plans may not cover Eliquis or may require substantial co-payments, making generic apixaban or other alternatives more financially viable. Prior authorization requirements can also delay treatment initiation, prompting consideration of immediately available alternatives.
Drug interactions and contraindications may necessitate switching to different anticoagulants. Patients taking certain medications that significantly interact with Eliquis, or those with specific medical conditions, may benefit from alternative blood thinners with different interaction profiles or monitoring requirements.
FDA-Approved Eliquis Alternatives
Generic Eliquis (Apixaban) – Bioequivalent Cost Savings
The FDA approved the first generic versions of apixaban on December 23, 2019, marking a significant milestone for cost-conscious patients. Generic apixaban contains the same active ingredient as brand-name Eliquis and must demonstrate bioequivalence, meaning it delivers the same amount of medication to the bloodstream at the same rate as the original.
Multiple manufacturers now produce generic apixaban, including Mylan, Teva, and Aurobindo Pharma. This competition has driven prices down considerably, with generic apixaban typically costing 60-80% less than brand-name Eliquis. Patients can expect to pay $100-$200 for a 30-day supply of generic apixaban, compared to $550-$600 for Eliquis.
The therapeutic equivalence of generic apixaban to Eliquis means patients can expect identical efficacy and safety profiles. The same dosing recommendations apply: 5 mg twice daily for most AFib patients, with dose reductions to 2.5 mg twice daily for patients meeting specific criteria including age ≥80 years, body weight ≤60 kg, or serum creatinine ≥1.5 mg/dL.
Rivaroxaban (Xarelto) – Once-Daily Convenience
Rivaroxaban, marketed as Xarelto by Bayer and Janssen, offers the convenience of once-daily dosing for most indications. Like Eliquis, Xarelto is a Factor Xa inhibitor that doesn’t require routine blood monitoring. The once-daily dosing may improve medication adherence, particularly important given that up to 25% of patients discontinue DOACs within the first year of treatment.
For atrial fibrillation, the standard Xarelto dose is 20 mg once daily with the evening meal. Patients with moderate kidney impairment (creatinine clearance 15-50 mL/min) receive a reduced dose of 15 mg daily. For DVT/PE treatment, patients typically start with 15 mg twice daily for 21 days, then continue with 20 mg once daily.
Cost-wise, Xarelto carries a similar price point to brand-name Eliquis, with 30-day supplies ranging from $500-$550. However, Bayer offers patient assistance programs and co-pay cards that can significantly reduce out-of-pocket costs for eligible patients. The convenience of once-daily dosing may justify the cost for patients who struggle with twice-daily regimens.
Dabigatran (Pradaxa) – Direct Thrombin Inhibition
Pradaxa (dabigatran) takes a different mechanistic approach as a direct thrombin inhibitor rather than a Factor Xa inhibitor. Manufactured by Boehringer Ingelheim, dabigatran directly binds to thrombin, preventing the conversion of fibrinogen to fibrin and subsequent clot formation.
The standard dose for AFib patients is 150 mg twice daily, with a reduced dose of 75 mg twice daily for patients with severe kidney impairment (creatinine clearance 15-30 mL/min). Pradaxa must be taken with a full glass of water and should not be crushed or opened, as this significantly increases bleeding risk.
A unique advantage of dabigatran is the availability of idarucizumab (Praxbind), a specific reversal agent that can rapidly neutralize dabigatran’s anticoagulant effects in emergency situations. This makes Pradaxa particularly attractive for patients at higher bleeding risk or those requiring urgent surgical procedures.
Pradaxa costs approximately $500-$530 for a 30-day supply, similar to other brand-name DOACs. The manufacturer provides patient assistance programs and co-pay cards to help reduce costs for eligible patients.
Edoxaban (Savaysa) – Simplified Dosing
Edoxaban, marketed as Savaysa by Daiichi Sankyo, represents another once-daily Factor Xa inhibitor option. The medication offers simplified dosing with fewer drug interactions compared to some alternatives, making it suitable for patients taking multiple medications.
For AFib patients, the standard dose is 60 mg once daily, reduced to 30 mg daily for patients with creatinine clearance 15-50 mL/min, body weight ≤60 kg, or concurrent use of certain P-glycoprotein inhibitors. Unlike some other DOACs, edoxaban should not be used in AFib patients with creatinine clearance >95 mL/min due to reduced efficacy.
Savaysa generally costs $480-$520 for a 30-day supply, positioning it competitively among DOAC options. The manufacturer offers patient support programs including co-pay assistance for commercially insured patients.
An important consideration with edoxaban is its metabolism through the liver. Patients with severe liver impairment should avoid this medication, and those with moderate liver disease require careful monitoring.
Warfarin (Coumadin/Jantoven) – Time-Tested Affordability
Warfarin remains the most cost-effective oral anticoagulant, with generic versions costing approximately $4 for a 30-day supply. As a vitamin K antagonist, warfarin has over 60 years of clinical experience and extensive research supporting its use across various patient populations.
The primary drawback of warfarin is the need for regular INR monitoring to maintain therapeutic anticoagulation levels between 2.0-3.0 for most indications. Patients typically require INR checks every 2-4 weeks once stable, with more frequent monitoring during initiation or dose adjustments.
Warfarin interacts with numerous medications and foods containing vitamin K, requiring patients to maintain consistent dietary habits and careful medication management. Despite these challenges, warfarin remains highly effective for stroke prevention in AFib and treatment of venous thromboembolism.
For patients who can successfully manage INR monitoring and dietary considerations, warfarin offers excellent anticoagulation at a fraction of the cost of newer agents. Many patients achieve stable INR levels and experience good quality of life on warfarin therapy.
Injectable Anticoagulants (Heparin, Enoxaparin) – Hospital and Transitional Use
Injectable anticoagulants like unfractionated heparin and low molecular weight heparins (such as enoxaparin/Lovenox) primarily serve specific clinical situations rather than long-term outpatient therapy. These medications are commonly used in hospital settings, for bridging therapy during warfarin initiation, or in patients who cannot take oral anticoagulants.
Unfractionated heparin requires continuous intravenous infusion with frequent monitoring of activated partial thromboplastin time (aPTT) levels. Enoxaparin can be administered subcutaneously once or twice daily and typically doesn’t require routine monitoring in patients with normal kidney function.
While these injectable options are not practical for most long-term anticoagulation needs, they play important roles in specific clinical scenarios and may be used temporarily while transitioning between oral anticoagulants.
Side Effects & Safety Profiles
Bleeding Risk Comparison – Clinical Trial Evidence
The landmark ARISTOTLE trial provided crucial safety data comparing apixaban to warfarin in AFib patients. Apixaban has demonstrated reduced bleeding risk compared to warfarin in clinical trials, but specific ARISTOTLE trial data is not available here for verification
Comparing bleeding rates across DOACs reveals important differences. Dabigatran shows higher gastrointestinal (GI) bleeding rates than warfarin, but direct comparisons of major bleeding rates across DOACs are not confirmed.
Gastrointestinal bleeding patterns differ among anticoagulants. Dabigatran shows higher rates of GI bleeding compared to warfarin, while apixaban demonstrates lower rates. Rivaroxaban and edoxaban show intermediate GI bleeding risks. These differences may influence anticoagulant selection for patients with prior GI bleeding history.
Other Common Adverse Effects
Beyond bleeding complications, anticoagulants can cause various other side effects that impact patient quality of life. Bruising represents the most commonly reported non-major bleeding symptom. While usually not medically significant, excessive bruising can cause cosmetic concerns and anxiety.
Dabigatran commonly causes GI symptoms, potentially due to its tartaric acid content. It particularly shows higher rates of dyspepsia, likely related to its tartaric acid formulation. Taking medications with food can help reduce these symptoms for most patients.
Dizziness and fatigue are reported but occur in 2–5% of users based on available data. These symptoms rarely require medication discontinuation but may affect daily activities.
Skin reactions, including rash and itching, occur infrequently but may necessitate switching to alternative anticoagulants. Drug-specific allergic reactions are rare but require immediate discontinuation and alternative anticoagulation strategies.
Cost Comparison & Coupons
Understanding the true cost of anticoagulant therapy requires examining both retail prices and available discount programs. In the U.S., generic apixaban is not yet widely available as of 2025, so most patients pay the brand-name price of $478–$600 for a 30-day supply, depending on pharmacy and coupon use. In Canada, generic apixaban is available for $70–$100 per month.
Related Post – Is It Safe to Buy Eliquis from Canada? A Complete Guide for Fixed Income Retirees in America
Xarelto and Pradaxa maintain similar pricing to brand-name Eliquis, with 30-day supplies costing $500-$550. Savaysa prices are slightly lower at $480-$520 monthly. Warfarin remains the most economical option at approximately $4 for a 30-day supply, though patients must factor in INR monitoring costs.
Manufacturer co-pay cards can significantly reduce costs for commercially insured patients. Bristol-Myers Squibb offers the Eliquis Co-pay Card, which can reduce monthly costs to as low as $10 for eligible patients. Similar programs exist for other brand-name DOACs, though eligibility requirements and benefit limits vary.
Patient assistance programs (PAPs) provide free medications for qualifying low-income patients. Each manufacturer operates separate programs with different income requirements, typically ranging from 200-400% of federal poverty level. These programs require annual reapplication and physician participation.
Discount card programs like GoodRx, SingleCare, and others can provide 10-80% savings on prescription medications, particularly beneficial for uninsured patients or those in Medicare coverage gaps. These programs work at most pharmacies and don’t require pre-qualification.
How to Switch Anticoagulants Safely
Transitioning to Warfarin – Monitoring Requirements
Switching from DOACs to warfarin requires careful planning and monitoring to maintain therapeutic anticoagulation while avoiding excessive bleeding risk. The transition typically involves overlapping anticoagulation with parenteral agents like enoxaparin until warfarin reaches therapeutic INR levels.
The process begins with discontinuing the DOAC and initiating warfarin at appropriate starting doses, typically 5-10 mg daily for most patients. Simultaneously, patients receive enoxaparin or another low molecular weight heparin until INR levels reach 2.0-3.0 on consecutive measurements at least 24 hours apart.
INR monitoring frequency during warfarin initiation requires daily checks for the first 3-5 days, then every 2-3 days until stable therapeutic levels are achieved. This intensive monitoring period typically lasts 1-2 weeks, after which patients can transition to routine monitoring every 2-4 weeks.
Patient education becomes crucial during warfarin transitions. Patients must understand dietary restrictions, drug interactions, and the importance of consistent INR monitoring. Many patients benefit from warfarin education classes or comprehensive counseling sessions.
Switching to Other DOACs – Timing Considerations
Transitioning between different DOACs requires attention to timing and renal function to maintain appropriate anticoagulation. The general principle involves discontinuing the current DOAC and initiating the new agent at the time of the next scheduled dose.
For patients with normal kidney function, the switch can typically occur 12 hours after the last dose of a twice-daily DOAC or 24 hours after a once-daily agent. Patients with impaired renal function may require longer intervals between medications to allow adequate clearance.
Renal considerations become particularly important when switching anticoagulants. All DOACs require dose adjustments for kidney impairment, but the specific criteria and dose reductions vary among agents. Creatinine clearance calculations guide appropriate dosing decisions.
Close monitoring during the transition period helps identify any bleeding or thrombotic complications. Patients should receive clear instructions about when to seek medical attention and how to manage minor bleeding episodes during the switch.
Natural & Dietary Alternatives
Ginger, Turmeric, Garlic – Limited Clinical Evidence
Natural supplements marketed for cardiovascular health often claim anticoagulant properties, but robust clinical evidence supporting their use as eliquis alternatives remains limited. Ginger contains compounds like gingerols that may inhibit platelet aggregation, but studies showing clinically significant anticoagulant effects are lacking.
Turmeric’s active compound curcumin demonstrates anti-inflammatory properties and may affect blood clotting in laboratory studies. However, the bioavailability of curcumin is poor, and human studies haven’t established therapeutic anticoagulant effects comparable to prescription medications.
Garlic supplements contain compounds that may influence blood clotting, but clinical trials haven’t demonstrated consistent anticoagulant effects. Additionally, garlic can interact with prescription anticoagulants, potentially increasing bleeding risk when used concurrently.
The lack of standardization in natural supplement preparations makes it impossible to ensure consistent dosing or effects. Unlike FDA-approved medications, dietary supplements don’t undergo rigorous testing for safety and efficacy. Patients considering natural blood thinners should discuss these options with healthcare providers and never discontinue prescribed anticoagulants without medical supervision.
Insurance, Patient Support & Saving Strategies
Navigating insurance coverage for anticoagulants requires understanding formulary restrictions, prior authorization requirements, and available assistance programs. Many insurance plans prefer generic medications or specific brand-name agents, requiring patients to try preferred options before covering alternatives.
State pharmaceutical assistance programs provide additional resources for eligible patients. Programs like PACE (Pharmaceutical Assistance Contract for the Elderly) in Pennsylvania and similar initiatives in other states offer prescription drug coverage for seniors and disabled individuals who don’t qualify for other assistance programs.
Medicare Part D coverage for anticoagulants varies by plan, with some plans requiring step therapy or prior authorization. The Medicare coverage gap (donut hole) can create temporary high out-of-pocket costs, making manufacturer assistance programs particularly valuable for Medicare beneficiaries.
Pharmaceutical company patient assistance programs typically provide the most comprehensive support for qualifying patients. Bristol-Myers Squibb’s Patient Assistance Foundation, Bayer’s Patient Assistance Program, and similar initiatives from other manufacturers can provide free medications for patients meeting income requirements.
Frequently Asked Questions
Is generic apixaban as effective as brand-name Eliquis?
Yes, generic apixaban must demonstrate bioequivalence to Eliquis, meaning it delivers the same amount of active ingredient to your bloodstream at the same rate. The FDA requires generic medications to have identical therapeutic effects as brand-name versions.
Can I switch between different blood thinners on my own?
No, switching anticoagulants requires medical supervision to ensure proper timing and dosing. Improper transitions can lead to dangerous blood clots or bleeding complications. Always consult your healthcare provider before making changes.
How much money can I save with anticoagulant coupons?
Savings vary significantly depending on your insurance status and the specific program. Manufacturer co-pay cards can reduce costs to $10-$25 monthly for commercially insured patients, while patient assistance programs may provide free medications for qualifying low-income individuals.
Are natural blood thinners safe alternatives to prescription medications?
Natural supplements lack the clinical evidence supporting prescription anticoagulants and aren’t appropriate substitutes for FDA-approved medications in patients requiring anticoagulation for conditions like atrial fibrillation or blood clots.
What should I do if I can’t afford my blood thinner?
Contact your healthcare provider immediately to discuss alternatives. Options may include generic versions, manufacturer assistance programs, state pharmacy assistance programs, or switching to more affordable alternatives like warfarin with appropriate monitoring.
How do I know which blood thinner is right for me?
The choice depends on multiple factors including your medical condition, kidney function, other medications, bleeding risk, and ability to comply with monitoring requirements. Your healthcare provider will consider all these factors to recommend the most appropriate option.
Conclusion & Next Steps
The landscape of eliquis alternatives offers multiple options for patients seeking effective and affordable anticoagulation. Generic apixaban provides the most direct cost savings while maintaining identical efficacy to brand-name Eliquis. Other DOAC alternatives like Xarelto, Pradaxa, and Savaysa offer different dosing schedules and safety profiles that may better suit individual patient needs.
Warfarin remains a highly effective and economical choice for patients who can manage INR monitoring and dietary considerations. The dramatic cost difference – approximately $4 versus $550 monthly – makes warfarin particularly attractive for uninsured patients or those facing high co-payments.
For patients who prefer to continue with Eliquis or generic apixaban due to their proven safety profile and convenience, exploring affordable pharmacy options becomes essential. When you’re ready to buy Eliquis at reduced costs, PrescriptionPoint.com offers significant savings on Eliquis and other anticoagulants, providing access to FDA-approved medications at substantially reduced prices. This trusted online pharmacy platform connects Americans with licensed pharmacies, ensuring medication authenticity while delivering meaningful cost savings that can make the difference between affording treatment and going without.
Patient assistance programs, manufacturer co-pay cards, and discount programs can significantly reduce the financial burden of anticoagulant therapy. Combining these resources with affordable pharmacy options like PrescriptionPoint.com often reveals multiple pathways to accessing necessary medications without compromising household budgets.
The decision to switch anticoagulants should always involve comprehensive discussion with healthcare providers. Factors including medical history, kidney function, drug interactions, bleeding risk, and lifestyle considerations all influence the optimal choice for individual patients. However, cost should never force patients to compromise on medically appropriate therapy when affordable alternatives exist.
Moving forward, patients should work closely with their healthcare teams to evaluate both clinical and cost considerations when selecting anticoagulants. Exploring resources like PrescriptionPoint.com for medication savings, while maintaining regular monitoring and open communication with providers, ensures safe, effective anticoagulation without financial hardship. The goal remains preventing dangerous blood clots while maintaining quality of life and financial stability through smart healthcare purchasing decisions.
References
- CDC.gov. (2025). Data and Statistics on Venous Thromboembolism
- Wikipedia.org. (2025). Pulmonary embolism
- CDC.gov. (2024). About Atrial Fibrillation
- VeryWellHealth.com. (2023). What Is Deep Vein Thrombosis?
- Bms.com. (2025). Key facts
- Accessdata.fda.gov. (2021). Prescribing Information
- Singlecare.com. (2025). What tier drug is Eliquis?
- Healthline.com. (2024). Is Eliquis Covered by Medicare?
- Singlecare.com. (2024). Eliquis interactions to avoid
- Tctmd.com. (2019). FDA Approves Two Generic Versions of Apixaban
- Brieflands.com. (2025). Pharmacokinetics and Bioequivalence of Two Formulations of Apixaban Tablets: A Double-Blind, Single-Dose, Crossover Study in Healthy Subjects
- Dataintelo.com. (2024). Apixaban API Market
- Singlecare.com. (2023). Eliquis generic availability, cost, and dosage
- Rxlist.com. (2021). Apixaban
- Janssenlabels.com. (2023). Patient Counselling Information
- Goodrx.com (2024). 7 Xarelto Side Effects You Should Know About
- Mayoclinic.org. (2025). Rivaroxaban (oral route)
- Wikipedia.org. (2025). Dabigatran
- Drugwatch.com. (2025). Blood Thinners.
- Pubmed.ncbi.nlm.nih.gov. (2016). Safety Signal Evaluation of a Risk of Syncope and Dizziness Not Related to Bleeding or Stroke in Direct Oral Anticoagulant-treated Patients
- Eurannallergyimm.com. (2019). Delayed hypersensitivity to new oral anticoagulants. Demonstration of cross reactivity for the drug category and definition of non-irritant concentrations for patch tests
- Singlecare.com. (2025). How much do blood thinners cost?
- Medicalnewstoday.com. (2023). Eliquis (apixaban) and cost
- Singlecare.com. (2025). Eliquis Coupons
- Goodrx.com (2025). Apixaban
- Ahajournals.org. (2020). Direct Oral Anticoagulant Use: A Practical Guide to Common Clinical Challenges
- Southdenver.com. Switching To and From Various Anticoagulants
- Gov.bc.ca. (2023). Direct Oral Anticoagulants (DOACs)
- National Library of Medicine. (2023). Functional bioactive compounds in ginger, turmeric, and garlic
- Jhrlmc.com. (2024). Exploring the Cardio-Protective Effect of Bioactive Compounds Present in Ginger, Garlic, and Turmeric
- Journals.sagepub.com. (2024). Efficacy of Phytopharmaca (Cinnamon, Turmeric, Ginger and Garlic) as an Adjuvant in Rheumatoid Arthritis Management: A Systematic Review and Meta-Analysis
- Sciencedirect.com. (2017). Old and new oral anticoagulants: Food, herbal medicines and drug interactions
- National Library of Medicine. (2023). Functional bioactive compounds in ginger, turmeric, and garlic
- Wiley.com. (2018). Effects of Garlic, Onion, Ginger, and Turmeric on Platelet Function
- Irjet.net. (2019). Health benefits and possible Risks of Turmeric, Garlic and Ginger: A short review
- Milliman.com. (2025). Potential impact of formulary restrictions on anticoagulants in the Post- Maximum Fair Price (MFP) Part D Market
- Ajmc.com. (2022). Formulary Restrictions and Stroke Risk in Patients With Atrial Fibrillation
- Medicalnewstoday.com. (2022). Xarelto vs. Eliquis
- Goodrx.com. (2023). Plavix vs. Eliquis: 7 Things to Know When Comparing These Blood Thinners
- Ti.ubc.ca. (2024). Apixaban is safer and more effective than rivaroxaban for non-valvular atrial fibrillation
- Fda.gov. (2020). 2019 First Generic Drug Approvals
India’s Historic Move to Make Drugs Affordable

Cancer is a word that no one wants to hear associated with them, no matter what kind of cancer. Historically, cancer treatments have been expensive, have bankrupted families, and caused a great deal of emotional and financial pain for the patient and the patient’s family.
There is a recent ray of hope, however. India is looking to put a stop to cancer, even for those who can’t afford treatment.
Nexavar (Sorafenib) Uses
Simply stated, this drug is used to treat two types of cancer — a type that starts in the kidneys, called “advanced renal cell carcinoma,” and a type of inoperable liver cancer, called “unresectable hepatocellular carcinoma.” This therapy slows the spread of cancer cells, and is in a class of drugs known as,
“Multikinase Inhibitors.”
This treatment, produced in brand name form by Bayer, is an expensive, patented treatment that costs approximately $5,600 US Dollars for a month’s worth of treatment. This price is often well out of the range of most people, especially those without insurance.
India’s Compulsory License Provision
The World Trade Organization (WTO) has a provision for something called a compulsory license, which means that any country can grant permission to a manufacturer to produce a patented medication without the consent of the owner of the patent. That means that a manufacturer can produce the same medication at a much lower cost.
In this case, India has been given permission to go ahead and manufacture Sorafenib for the treatment of liver and kidney cancer, which is a serious health crisis throughout the country. Under this compulsory license, the country’s manufacturers will be able to produce generic Nexavar for only $180 cost for a month’s supply. That’s $5,420 US Dollars LESS than the brand price. This means that just about anyone could afford cancer treatment.
Cancer Treatment at a Much Lower Cost
This huge cost-savings is a big relief for many people facing kidney or liver cancer. They will not have to decide between life-saving treatment or basic life needs. At a cost difference of $65,040 per year, cancer treatment will be suddenly attainable by a larger population. This is exciting news — not only for an effective cancer treatment, but for an effective cancer treatment that most people actually can afford.